Castor oil for dry eye? Demodex?
Castor oil has a long and ancient history as a traditional remedy for skin, scalp and hair ailments, and internally for gastrointestinal and reproductive applications. It is even mentioned in herbal medicine lists on papyrus from ancient Egypt.
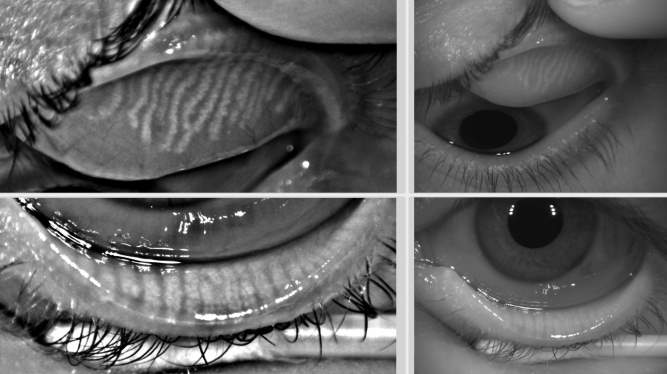
Today, castor oil continues to appear intermittently in online searches for natural treatments for blepharitis, so we’ve decided to study its effects in relation to dry eye, specifically with respect to anterior blepharitis and Demodex mites, and examine its likely mechanisms of action, in a scientific manner.
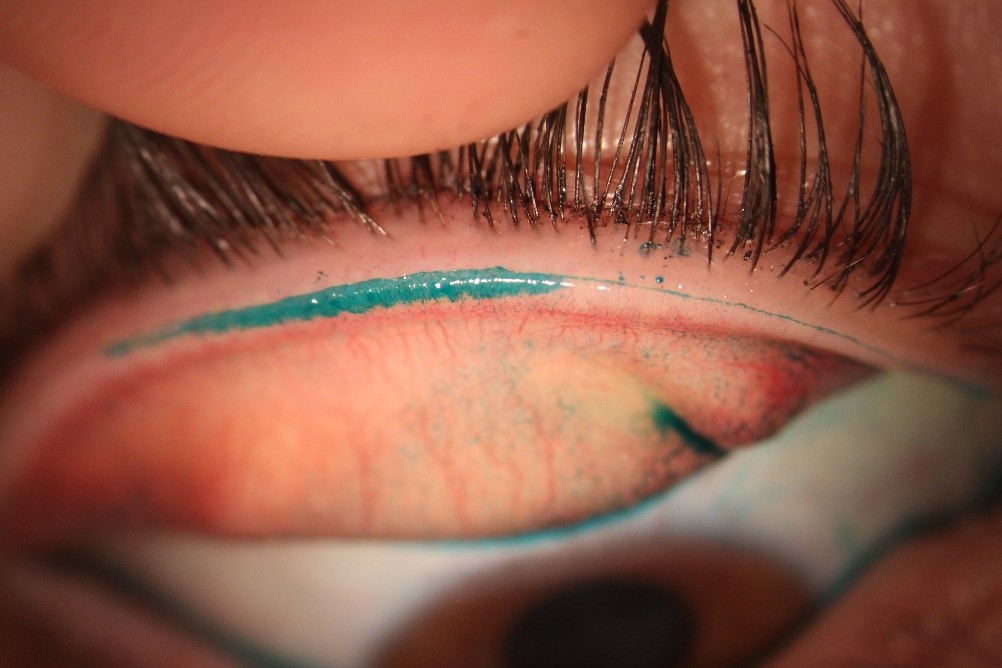
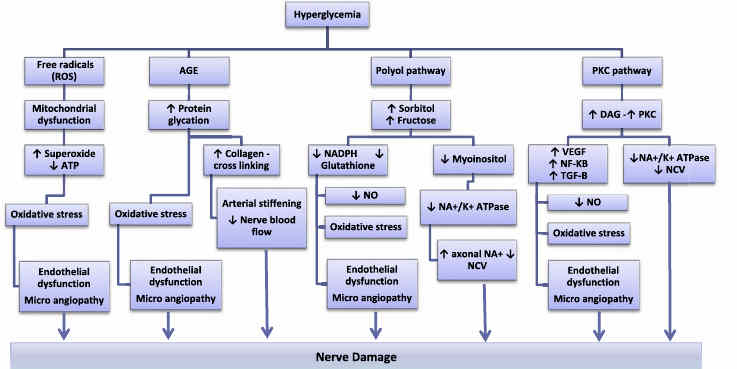
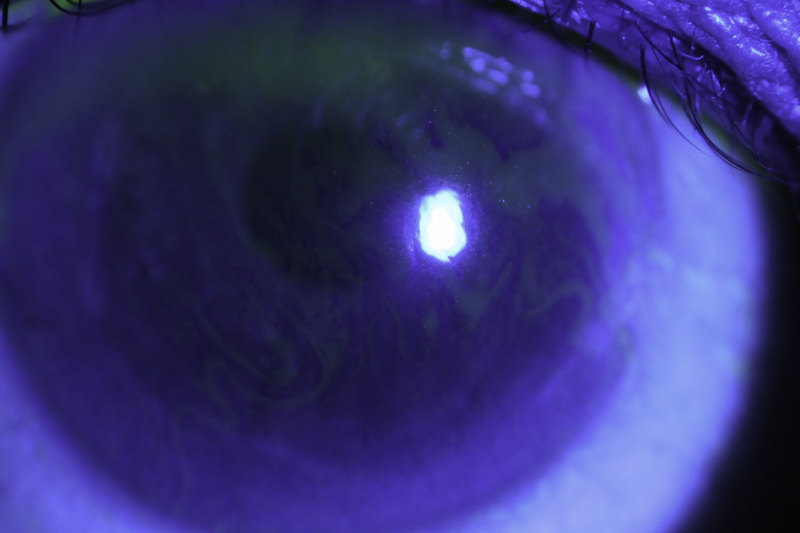
Castor oil’s main constituent is ricinoleic acid, which has a number of properties applicable to the different facets of the pathophysiology of blepharitis and dry eye. It is an emollient, anti-inflammatory, anti-microbial, anti-oxidant, and a surfactant with lipid layer-forming abilities, so it spreads across the tear film in a thin layer. It penetrates the lash follicles and there is every reason to suspect it might interfere with the physiology of Demodex mites, rather like tea tree oil.
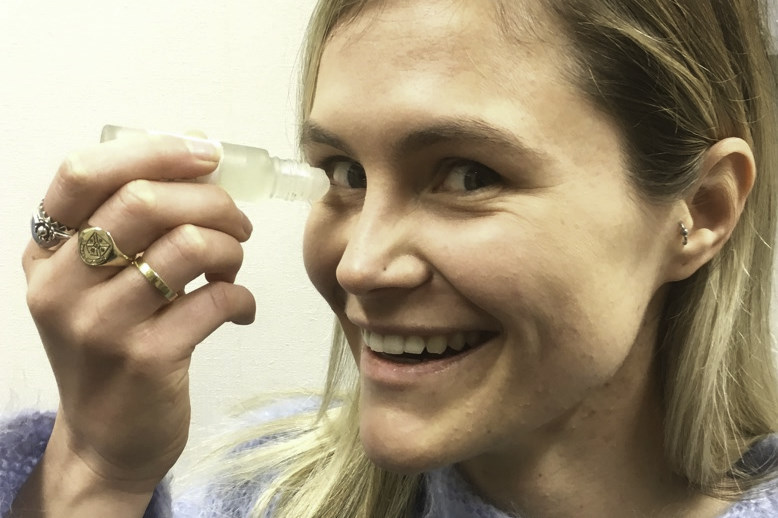
We are employing a unique rollerball application method, which ensures application of a thin film close to the lid margins. The hypothesis is this may have some therapeutic benefit in controlling blepharitis and Demodex, along with the possibility that a small degree of ingress into the tear film will enhance the lipid layer and could potentially address lipid layer deficiency which leads to dry eye symptoms associated with blepharitis.
Under the guidance of Associate Professor Jennifer Craig, we are conducting a prospective, randomised, investigator-masked trial of topically-applied castor oil for blepharitis as an optometry honours research project. This is being conducted by Part V students, Marna Claassen, Lauren Curd and Alice Jackson, who are recording a range of subjective and objective parameters to elicit symptomatic and biometric changes of the eyelids and tear film, including changes in ocular surface inflammatory biomarkers. We are excited to find out, when the data are unmasked at the conclusion of the study, whether a one-month application period has resulted in improvements in these parameters and lower titres of inflammatory markers. If so, this could infer long-term benefits with respect to minimising ocular surface inflammation and reducing the incidence of dry eye in blepharitis patients.
We are currently recruiting for this study. For more information and to check eligibility please call or text us on 022 EYE PAIN.
Dr Emma Sandford is a GP in the Bay of Plenty and an honorary academic, and Grant Watters is an optometrist and researcher at the University of Auckland.