CMDHB: more help needed
Four Counties Manukau District Health Board (CMDHB) ‘mega-clinics’ saw more than 550 patients, but there is still more to be done, said Dr Simon Dean, CMDHB ophthalmology clinical leader.
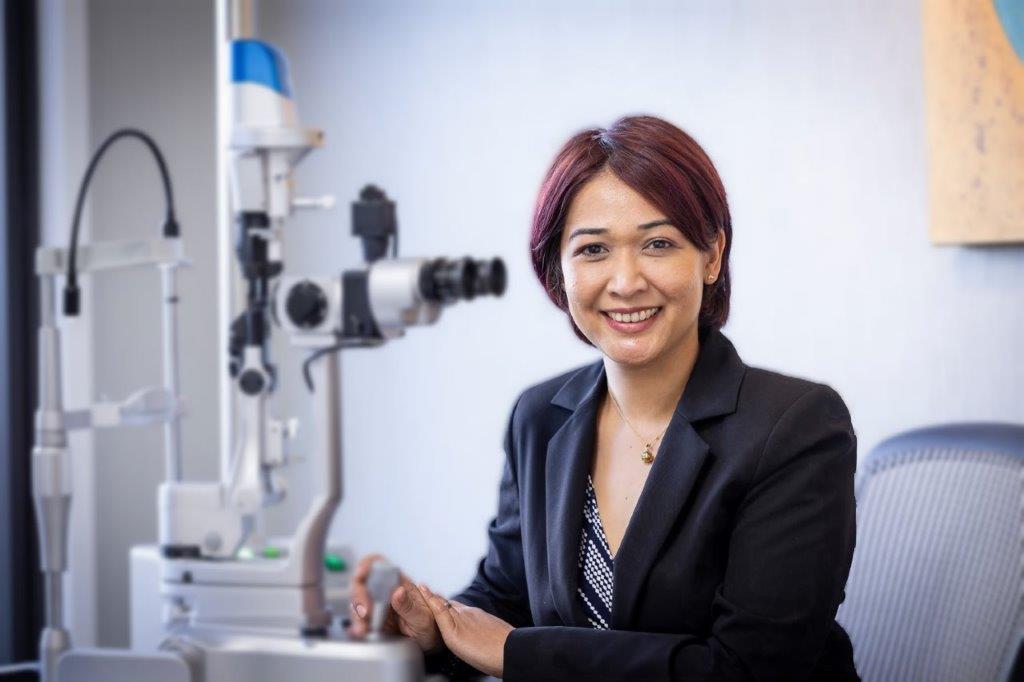
Answering CMDHB’s plea for help, the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) ran a series of eye care mega-clinics in May and June for high-risk patients. Eighteen ophthalmologists and 19 ophthalmic nurses and technical staff from across New Zealand answered the call and saw at-risk patients with medical retina, anterior segment and paediatric eye disorders. An audit was also performed at each of the clinics to identify cases of vision loss due to delayed follow-up so they can be investigated by the CMDHB.
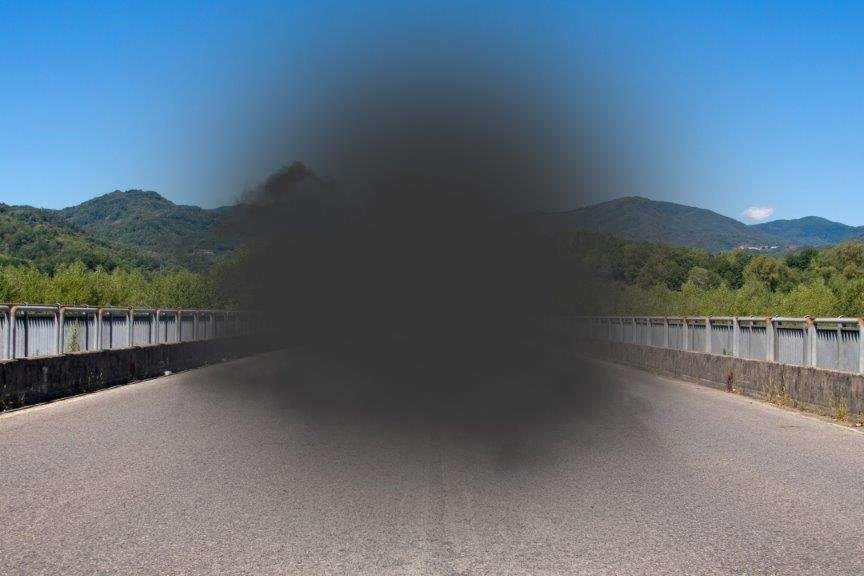
“The data gathered so far suggests a number of patients have had significant visual loss from waiting too long,” said Dr Dean. “The only way to reduce the risk is to see everyone who is overdue, but we just don’t have the resources to do this in Counties, and this is not just us but a common problem in eye clinics across New Zealand.”
The advent of treatments for age-related macular degeneration (AMD) has seen a huge increase in clinic visits nationally but so far, no tangible increase in resources to cope with the demand, he said. “Eye clinics across New Zealand are thinking outside the box to meet demand, but the reality is thresholds for normal daily eye clinic work such as cataracts, pterygium, etc. are rising. This is resulting is a stockpiling of pathology in the community and is already impacting on the complexity of cases managed in the eye clinics, further reducing throughput with disease being seen in later stages than previously and being more difficult, if not impossible, to manage.”
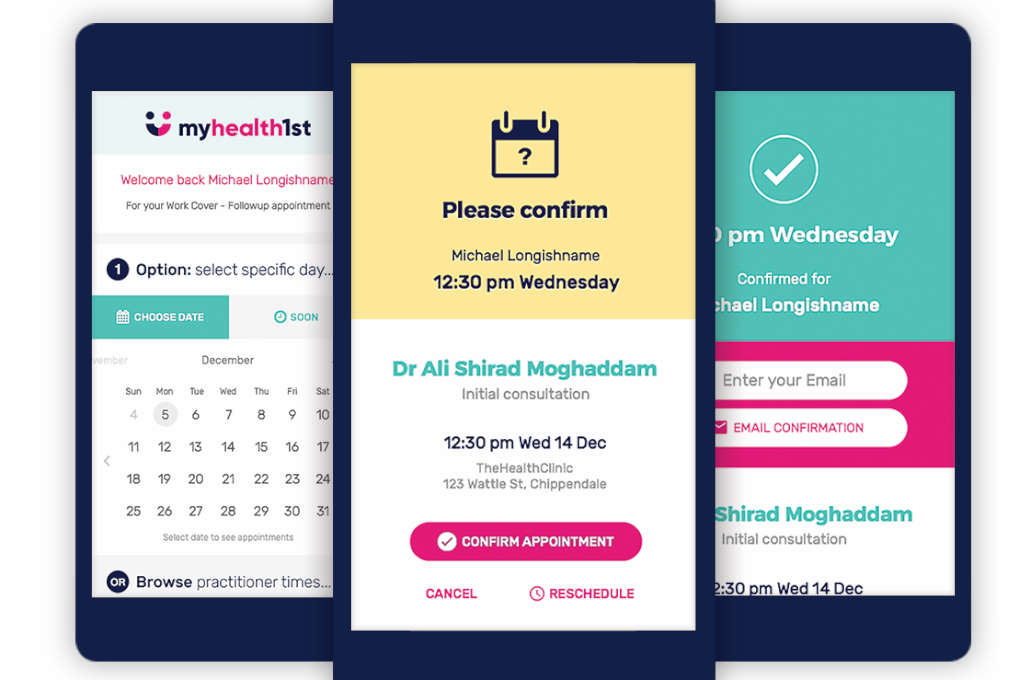
The management of patients who were booked, but did not attend, and clinical documentation were among other issues also identified as requiring review in CMDHB. The South Auckland-based DHB has committed to the Auckland Regional Ophthalmology Plan, which aims to rationalise ophthalmology services across the three Auckland DHBs, and a memorandum of understanding with RANZCO, which will lead to an overhaul of its systems and the adoption of new national guidelines* for treating AMD and an ‘acuity Index’ for prioritising follow-up appointments. But there’s still so much more that needs to be done, said Dr Dean.
“We need to significantly increase staffing (at CMDHB). We have been on the risk register since 2009. We also need to double our clinic size and theatre access to match Auckland DHB. Some DHBs, such as Counties Manukau, are financially compromised as we serve a greater population than the census figures would suggest, and we are funded based on the population size we serve.”
The success of the clinics in helping to clear a big chunk of the backlog in the region was heralded, however, by those who took part, RANZCO and staff at the Counties Manukau Eye Clinic.
The mega-clinics have been great for so many of our patients and helped us to identify high-risk patients who need close, on-going care,” said Krishnee Naidoo, clinical nurse manager.
Another important benefit of the clinics has been the exchange of ideas and treatment protocols between ophthalmologists, nurses and technical staff from different DHBs, which has been “invaluable,” said Terri England, CMDHB service manager for ophthalmology.
For previous story on Counties Manukau initiative, see this story.
For more about the AMD Guidelines, see this story.