DSAEK, DMEK, epithelium-off crosslinking and blepharitis treatments
Efficacy and safety of DMEK versus DSAEK: a systematic review and meta-analysis
Saiqun Li, Liangping Liu, Wei Wang, Ting Huang, Xingwu Zhong, Jin Yuan, Lingyi Liang
PLoS One. 2017; 12(12): e0182275.
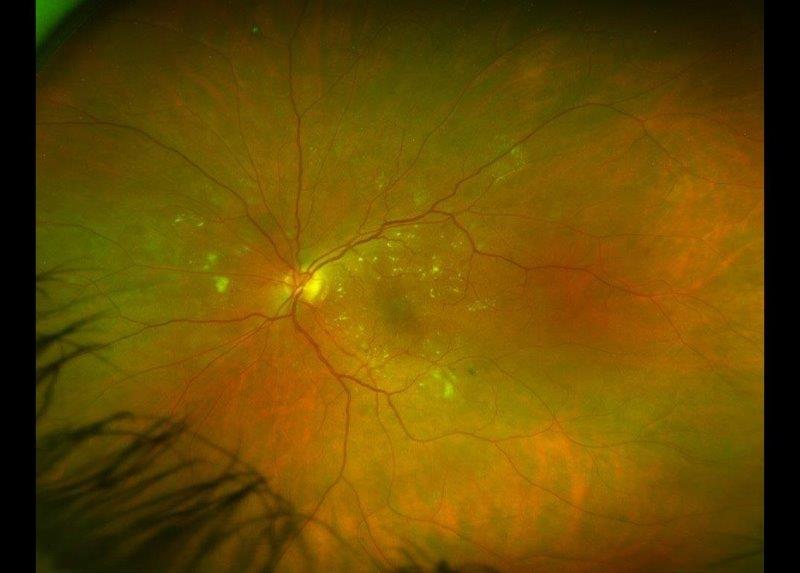
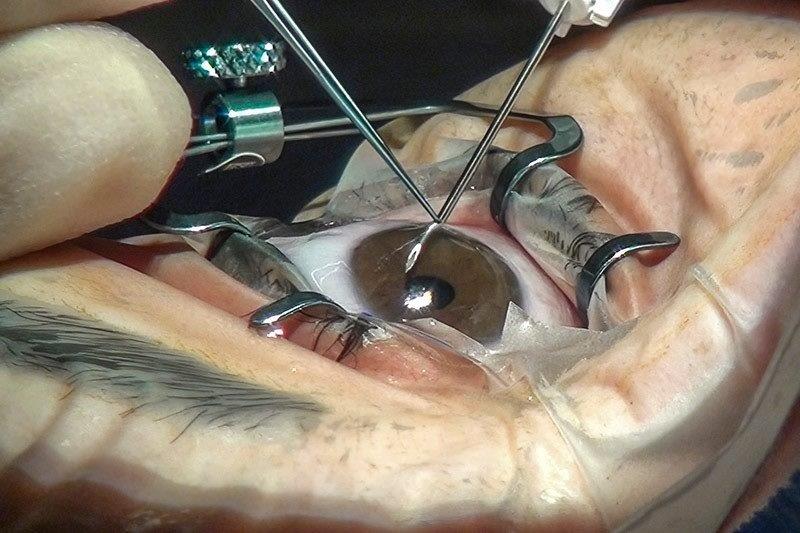
The surgical management of corneal decompensation has traditionally been with full thickness corneal transplantation or penetrating keratoplasty (PK) and more recently with lamellar transplantation techniques such as Descemet stripping automated endothelial keratoplasty (DSAEK), in which the Descemet’s membrane endothelial complex is transplanted with a sheet of stroma, and Descemet’s membrane endothelial keratoplasty (DMEK), in which the Descemet’s membrane endothelial complex is transplanted in isolation and attached in a suture-free method through gas tamponade.
In this meta-analysis, the authors evaluated 19 published articles comparing the outcomes of DSAEK and DMEK. The overall pooled estimates demonstrated a significantly superior post-operative best corrected visual acuity, a comparable endothelial cell density, and an increased graft detachment rate in the DMEK group compared with the DSAEK group.
Comment:
Endothelial keratoplasty is now the gold standard procedure for endothelial disease comprising 31% of corneal transplants performed in New Zealand in 2015. There is now increasing evidence to suggest that whilst technically more challenging, DMEK surgery provides better visual outcomes following surgery compared to more traditional DSAEK surgery, but further surgical refinements are required to shorten the learning curve and improve potential intra-operative and post-operative complications. Results of the currently running, multicentre, randomised clinical trial comparing DSAEK and DMEK are keenly awaited.
Patient satisfaction with epithelium-off corneal crosslinking
Price M, Feng M, Price F
J Cataract Refract Surg. 2018 Mar 28
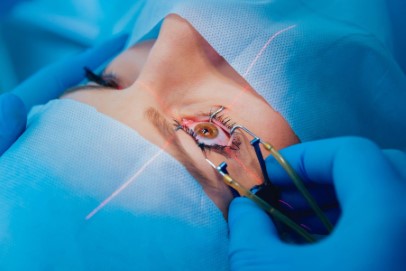
Crosslinking is the creation of bonds that connect one polymer chain to another. Corneal collagen crosslinking (CXL) is a technique used to strengthen corneal tissue utilising riboflavin (vitamin B2) as a photo-sensitizer and ultraviolet-A (UVA) to increase the formation of intra and inter-fibrillar carbonyl-based covalent bonds through the process of photo-polymerisation.
In this article, the authors evaluate the satisfaction rate of 448 patients after a mean period of 3.5 years following epithelium-off CXL. The mean satisfaction score was 8.8 ± 1.7 (SD) on a scale of 1 (would not recommend CXL) to 10 (definitely would recommend) among those treated for keratoconus. The authors also demonstrate that 93% of patients felt that the treatment halted the progression of the disease with younger patients reporting a higher efficacy rate. Regarding vision, 87% reported an improvement or stability of their vision following treatment. Only 1.7% of the 644 eyes treated required keratoplasty.
Comment:
Keratoconus is a debilitating condition with a disproportionately high-impact on public health resources and vision specific quality of life. CXL has revolutionised the management of keratoconus in recent years by effectively stabilising the underlying ectatic process and in some cases reversing the disease as quantified by key topographic, refractive and visual outcomes. More than a decade after being introduced, this minimally invasive treatment modality is now fulfilling the promise of treating keratoectasia at an earlier stage, preventing the morbidity associated with disease progression and precluding the need for the more invasive keratoplasty procedure. This article demonstrates that CXL is viewed by patients as effective in halting the progression of their ectatic disease and also stabilising or improving their vision.
Randomized double-masked trial of eyelid cleansing treatments for blepharitis
Sung J, Wang MTM, Lee SH, Cheung IMY, Ismail S, Sherwin T, Craig JP
Ocul Surf. 2018 Jan;16(1):77-83.
Blepharitis is complex ocular disorder characterised by an imbalance in ocular flora, meibomian gland dysfunction and eyelid/ocular surface inflammation. Blepharitis is one of the most prevalent ocular disorders encountered by eye care professionals. In this randomised, double-masked trial, the authors compared the efficacy of two lid hygiene techniques by asking patients to use a commercial eyelid cleanser in one eye and conventional lid hygiene technique using diluted baby shampoo in the other. The results showed that whilst both treatments reduced the patient reported SPEED symptom score and improved lash crusting and trichiasis, the eyelid cleanser was the preferred treatment of choice for most patients (53% vs. 9%, p < 0.001). The cleanser also resulted in superior improvements in clinical features such as tear lipid layer and ocular surface inflammatory markers such as MMP-9 expression. In a concerning finding, the authors reported that baby shampoo treatment was associated with adverse outcomes such as meibomian gland capping and MUC5AC expression (a marker of goblet cell density and function within the conjunctiva).
Comment:
Blepharitis is a common ocular disorder that can lead to significantly altered quality of life. All eye care professionals are well aware of the challenges associated with satisfactorily treating patients with this chronic disease. This article provides an insight into the potential advantages of using commercial cleansing products over traditional methods of lid hygiene and highlights the need for further studies looking into the effects of using household products such as baby shampoo on the ocular surface.
About the author:
Dr Mo Ziaei has undergone quadruple fellowship training in the field of cornea, ocular surface disorders and anterior segment surgery at Moorfields Eye Hospital, London, and New Zealand National Eye Centre, Auckland. He is an honorary senior lecturer at the University of Auckland and a cornea and sight correction specialist at Re: Vision clinic and surgery centre.