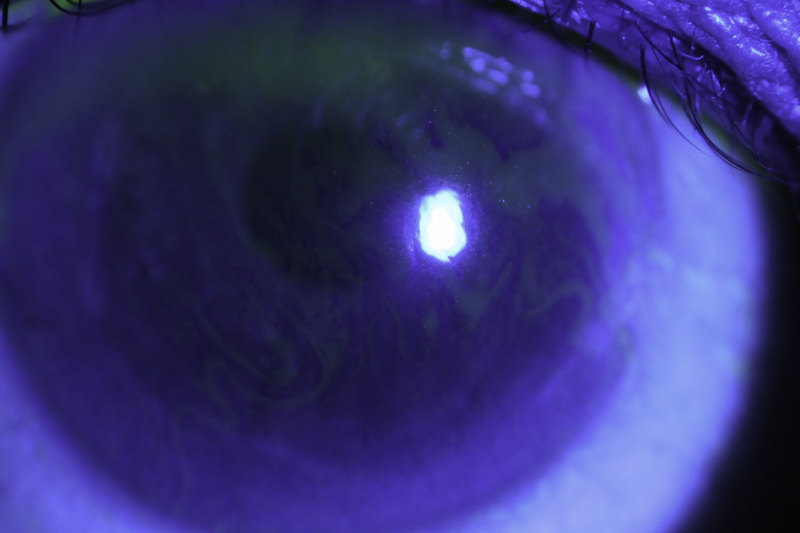
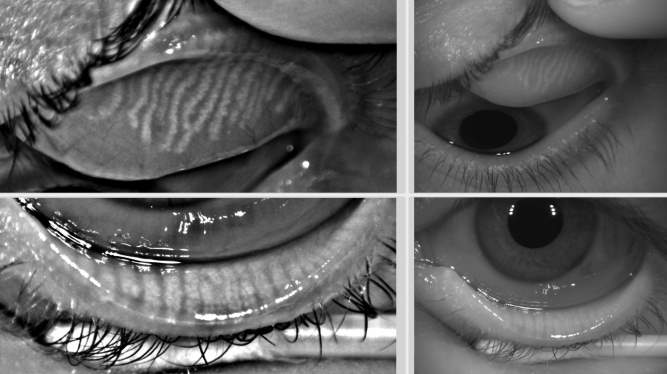
Fluorescein and tear film stability assessment
Tear film stability measurement is an integral component of the assessment of dry eye disease. Although ocular instillation of sodium fluorescein via impregnated strips is conventionally used to visualise tear film breakup, it is also recognised to destabilise the tear film, reducing stability measurements obtained. In recent years, however, automated, non-invasive measurement techniques have become available and are recommended by the global consensus TFOS DEWS II dry eye diagnostic criteria, in preference to fluorescein breakup time measurement.
Two recent studies conducted by the University of Auckland Ocular Surface Laboratory (OSL) compared tear film stability measurements obtained by the traditional fluorescein and contemporary non-invasive methods.
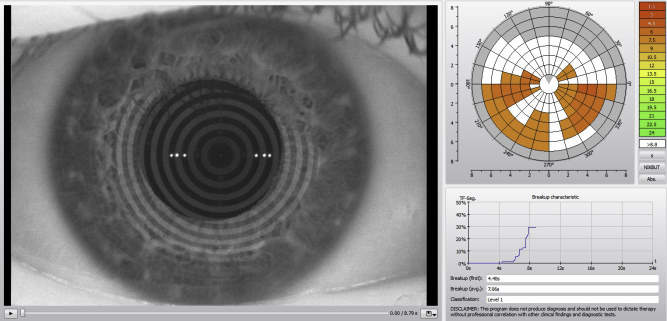
The first, recently published randomised crossover study of 74 participants (including 37 dry eye patients and 37 age, gender and ethnicity-matched healthy participants) compared measurements obtained by the conventional fluorescein method with those from an automated non-invasive corneal topographer (Oculus Keratograph 5M) and evaluated their respective discriminative ability in detecting symptomatic dry eye.
Automated non-invasive keratograph breakup time (NIKBUT) measurements were found to be significantly longer than fluorescein breakup time in both dry eye patients and healthy participants. The optimal diagnostic cut-off for NIKBUT was also longer, at 9 seconds, than the best cut-off point for the fluorescein breakup time, which was shown to be 5 seconds. Furthermore, NIKBUT measurements had better discriminative ability, sensitivity and specificity than the conventional fluorescein breakup time test.
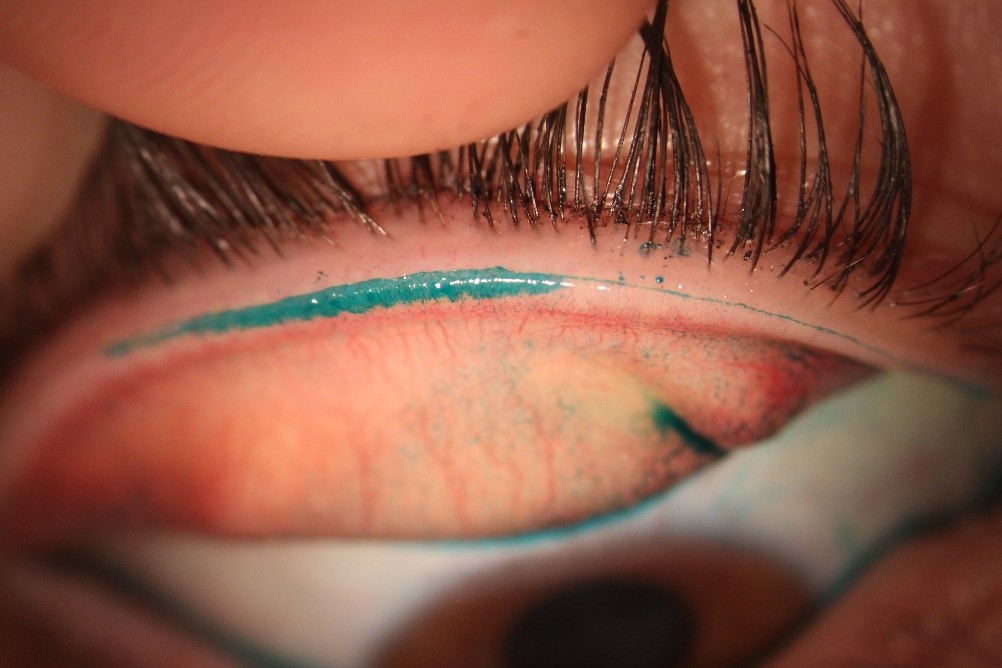
The other prospective crossover study of 41 participants compared tear film breakup time measurements obtained non-invasively, with minimal fluorescein instillation (1L), and conventional fluorescein strips (15-30 L). The results showed that breakup time values measured with conventional fluorescein instillation were significantly shortened, while those obtained with tiny amounts of fluorescein instillation compared much better to non-invasive measurement techniques.
The findings suggest, that where non-invasive measures are not available, we can reduce the destabilising impact of fluorescein on clinical measurements of tear film stability by minimising the volumes we instil!
References
Wang MT, Craig JP. Comparative Evaluation of Clinical Methods of Tear Film Stability Assessment: A Randomized Crossover Trial. JAMA Ophthalmology. 2018;136(3):291-294.
Mooi JK, Wang MT, Lim J, Müller A, Craig JP. Minimising instilled volume reduces the impact of fluorescein on clinical measurements of tear film stability. Contact Lens Anterior Eye. 2017;40(3):170-174.
By Dr Michael Wang, Dr Jennifer Mooi, Joevy Lim, Dr Andreas Müller and A/Prof Jennifer Craig