From practitioner to patient
When South Island optometrist John Veale hopped on a plane recently to Rarotonga, for what was perhaps his 40th trip with the NZ Aid eye team, he expected to see a few urgent medical cases. He didn’t expect to be one himself!
However, as the crew closed the aeroplane door and taxied down the runway, Veale, a well-known low vision patient advocate, noticed his sight was blurred and he had an unusual visual disturbance in his left eye.
“There were no flashing lights or floaters, or a wavy curtain, just a small triangle in my left nasal quadrant with a curved boarder,” he explains. “If I looked straight ahead and moved my hand toward my nose, my hand disappeared like magic. When I looked out the window with my good eye covered, I could see things but there was a distinct black edge with an orange boarder in that nasal quadrant.”
For anyone, these symptoms would have been disturbing, but Veale’s unease was compounded by the fact he knew exactly what was going on – a retinal detachment.
“I’ve referred many a detached retina in my time. They usually turn up in the practice on a Friday afternoon and I send them straight off to hospital, but here I was watching my own retina detaching, trapped on a four-hour flight.”
As soon as Veale got off the plane he rang Dr Jo Sims in Auckland, an ophthalmologist he knows well from their voluntary work together in the Cook Islands.
“I said, ‘Hi Jo, I’m in Raro’ and I have a detached retina. She said, ‘get them on the next flight down here now’. I cleared my throat and said, ‘Jo, it’s my retina.’ There was total silence from her end of the line.”
Once she had composed herself, Dr Sims told Veale he needed to see an ophthalmologist fast, but the next flight back to Auckland wasn’t until the next day.
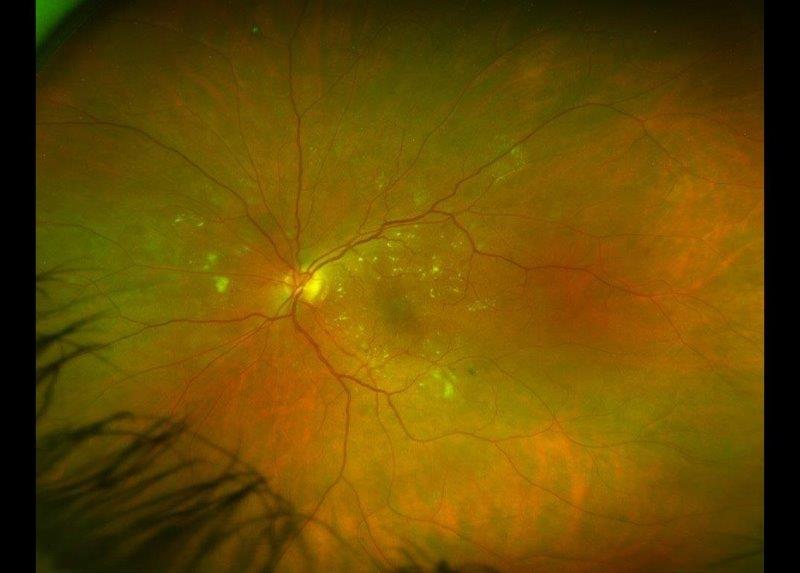
“My biggest fear was that this detachment was macula off,” says Veale. “As the day went on I slowly watched the boarder in my nasal quadrant move upwards. The retina was drifting down. I was watching it slowly peeling off.”
Veale did what I think most of us would do if trapped in this terrifying situation. He went to the pub!
By the time Veale got back to Auckland 24 hours later, he had very limited vision in his left eye. Dr Sims dilated him and did an OCT scan and confirmed his macula was off.
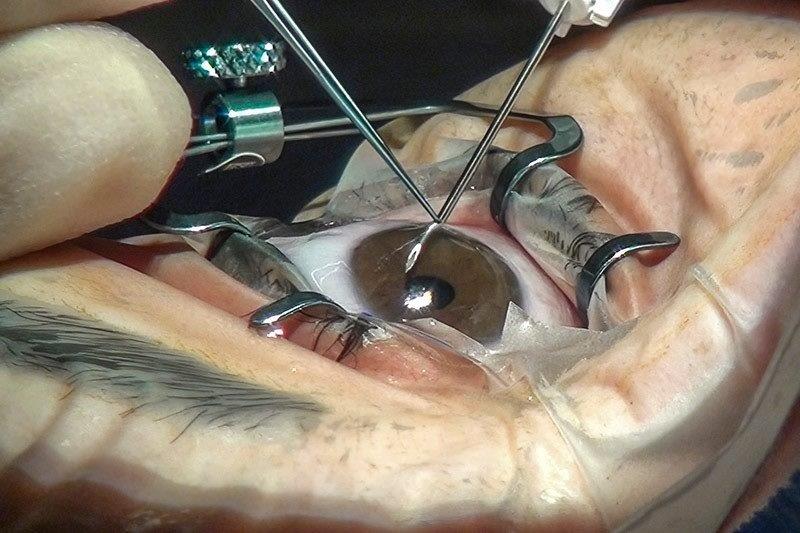
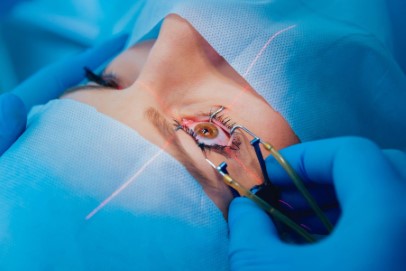
“I wasn’t happy,” says Veale. “I flew straight to Christchurch and someone drove me directly to the hospital. I’ve worked in the eye department there for about 30 years. Everyone knew me. Dr Jim Borthwick came in, fresh from a conference overseas, and operated around 8.30pm.”
Veale then describes the 10 days of absolute boredom as he lay on his side, gas pushing his retina up in the back of his eye. “I am officially the world’s worst patient,” he laughs. “My son brought me movies but I was too miserable to watch them. I couldn’t read. I hadn’t realised before that, that my left eye starts reading and my right eye doesn’t kick in until half way across the page.”
Immediately after surgery it was like looking through Vaseline, he says. “The bubble of gas starts off looking like the size of a medicine ball. It slowly shrank over 10 days to the size of a marble but bounced around in my eye as I moved. It was very disconcerting.”
Veale was one of the first optometrists in New Zealand to have LASiK about 25 years ago. Clear vision is exceptionally important to him so, as time went on, he felt unhappy about the vision recovery in his eye.
“I noticed the image was slightly smaller in the left eye than in the right and there was a bit of a distortion on the Amsler chart. I’d also discovered, I had three mini scotoma about 5 – 10 degrees out from the centre of the macula by using my own visual field test, and my contrast sensitivity test, normally level 13, was at level 10.”
When he tried to park his car, he would end up about two metres from the curb, and if he went inside wearing photochromatic lenses or got up in the night, he couldn’t see out of the left eye at all.
“About three weeks later I went to see Dr Sean Every,” says Veale. “He took a look and said Dr Borthwick did a really good job, but unfortunately my retina was splitting further over. So, I went back to the hospital for more surgery and ended up on my side for another 10 days, going barking mad.”
That second time round, Veale had pan-retinal lasering.
“You’re awake all the time, quite lucid. I had over 300 laser zaps. Hopefully that macula is not coming off again. It’s quite an experience.”
Veale, who has no plans to slow down despite the detachment, is in the middle of selling his Merivale practice so he can focus on other projects. Although he can make jokes about it now, he admits his sudden experience in the patient chair was quite frightening and illuminating.
“We always knew retinal detachment was an emergency – if you’re having a heart attack you don’t wait a week. The surgery has improved out of this world. Twenty years ago, they used to put a buckle on the eye, it was major surgery that caused ongoing problems. The results today are amazing. My vision is about 85% now in the affected eye and apparently that will continue to improve.”