Glaucoma Symposium 2018
An upbeat entrance through a high-tech trade fair was the welcome for this year’s glaucoma New Zealand symposium at Alexandra Park in Auckland. A record number of nurses and ophthalmic technicians, and even one GP, turned up as part of the 120-strong delegate list to hear talks and case studies from a strong line-up of 20 speakers.
Glaucoma’s impact
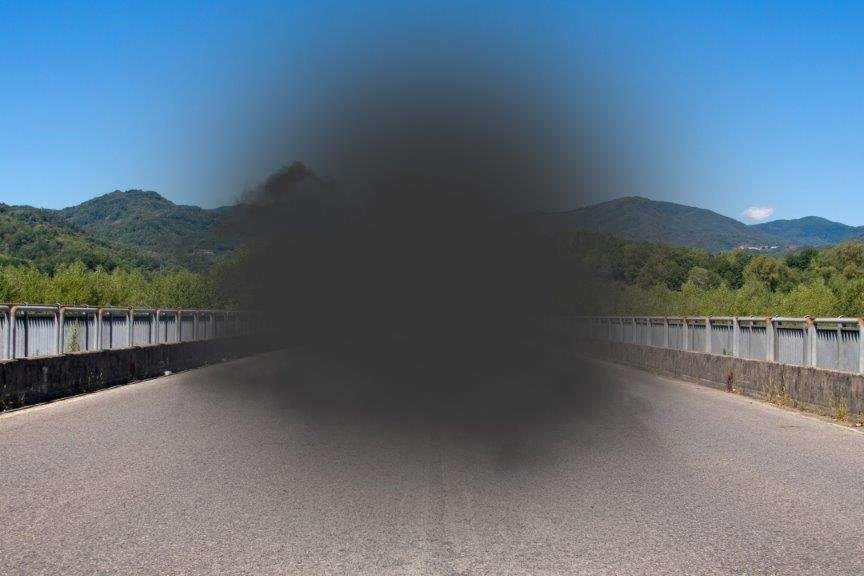
First up was keynote speaker Dr Simon Skalicky, a senior clinical lecturer at the University of Sydney and Melbourne and a glaucoma specialist at the Royal Victorian Eye and Ear Hospital, who discussed glaucoma’s effect on the quality of life. He reviewed research advances and clinical insights to help us understand when and how glaucoma becomes a disability. By translating the visual field into meaningful daily activities, we can improve the patient-clinician relationship and compliance to medication regimes, he said, and it helps guide further research into detection, monitoring and treatment.
High-quality questionnaires are essential for good patient outcomes, with too many focusing only on visual function and not addressing psychometric function, continued Dr Skalicky. The ideal patient-reported outcome measures (PROM) include classical validation, test-retest criteria and convergent and divergent validity. Current visual function tests include challenging obstacle courses or difficult visual tasks, such as asking the subject to find a hidden red box.
Skalicky also looked at ocular surface disease in glaucoma, a multi-factorial problem affecting 20-59% of patients. Preservatives impact negatively on the ocular surface, increasing inflammation and influencing goblet cells, osmolarity, eyelid position and abnormalities. Some preservatives (such as polyquad) may be better, but the overall eye drop load is important to consider. Eye drops without preservatives may have an important role in the future, but Dr Skalicky recognised the lack of them on the market currently.
Glaucoma nuts and bolts
Within the Nuts and bolts of glaucoma session, Dr Hussain Patel tackled When does a visual field defect concern me? Is the visual field test reliable? While there’s no hard and fast cut-off for fixation losses, false negatives and positives, these need to be carefully considered, he said, adding how important it is to check patient details and refraction. Could the visual field defect be due to artefacts? Think about taping the eyelids and watch out for the tell-tale ‘clover-leaf pattern’ indicative of fatigue. Is the defect repeatable? And, does the defect match the optic nerve defect? Dr Patel urged us to think of any other pathology that could cause this defect and, having considered all the above questions, decide for ourselves how concerning a visual field defect could be. “Overall, I am very concerned when a defect is progressing, involves central fixation or respects the vertical midline,” he surmised.
Optometrist turned consultant ophthalmologist Dr Divya Perumal refused the lectern, instead striding out to engage with the audience on angle closure. Presenting an image-rich presentation, she discussed the definitions of primary angle closure (PAC), PAC suspects and PAC glaucoma. Despite advances in anterior OCT imaging - including swept source, giving a 300° view, and ultrasound biomicroscopy, the only way to image the ciliary body - gonioscopy is still the gold standard. The mechanism of angle-closure is also important, said Dr Permual, explaining that while pupil block is easily fixed with a laser periphery iridotomy, other mechanisms such as ciliary block, lens mechanism or retro-lens mechanism may require a different treatment approach.
Perumal introduced the SImPle approach – an acronym for angle closure treatment - S for structure; I for irido-trabecular contact - if present, is it reversible? Consider whether it’s appositional vs synechiae, she said. While P stands for plateau iris, pigment, prominent iris processes and peculiarities. Using flow charts, Dr Perumal demonstrated when to intervene with each treatment after answering if the scleral spur was visible.
Dr Sonya Bennett outlined two syndromes seen more in optometry than in ophthalmology: pseudoexfoliation syndrome and pigment dispersion syndrome (PDS); signs for the latter being dense trabecular meshwork pigmentation, mid-peripheral iris transillumination defects and pigment deposition on the corneal endothelium. Some light irises may have transillumination, but in the absence of the other two signs it is not PDS, she said. Pseudoexfoliation syndrome, an age-related systemic syndrome, is characterised by white flaky material on various anterior ocular structures and has several systemic associations such as myocardial infarction.
Dr Graham Reeves ended the ‘nuts and bolts’ section with a fun, interactive session entitled, The great OCT glaucoma quiz. This reminded us about the use of the disc damage likelihood scale (DDLS), which is preferable to cup-disc ratio, and some of the pitfalls of OCT. Dry eyes, small pupils, cataract, asteroid hyalosis, vitreo-retinal junction abnormalities and myopia may all affect the quality of the scan, so look at the absolute nerve fibre layer loss, he said.
New concepts in glaucoma
Hawke’s Bay ophthalmologist Dr Alex Buller shared the outcome of his region’s shared-care glaucoma scheme, where optometrists examine patients in the community, but are paid $130 by the hospital for doing so.
Keynote speaker Dr Skalicky then presented on arguably the “hottest topic in glaucoma right now” – minimally invasive glaucoma surgery (MIGS), including the iStent, Cypass, Hydrus and Xen. These relatively new devices give consultants an array of options that sit between the least invasive techniques - selective laser trabeculoplasty (SLT) and eye drops - and more invasive options like filtration surgery. Cypass and iStent are often done at the same time as cataract surgery and may reduce the need for filtration surgery, he said, while the Xen gel implant is minimally disruptive with no incisions in the conjunctiva or sclera. SLT and eye drops are the safest techniques, but have limited impact on intraocular pressure, and trabeculoplasty is the least safe, but lowers eye pressure very well, he added.
Wellington ophthalmologist Dr Jesse Gale discussed the fascinating topic of rescuing retinal ganglion cells. Usually glaucoma is thought of as a one-way street - the nerve fibre layer dies and the visual field goes. But there are some cells that are “sick, but not yet dead,” he said and detecting these stressed or dysfunctional cells could have many positive applications for glaucoma patients.
Next Dr Jay Meyer answered the question, Doc, what else can I do for my glaucoma? This reviewed the evidence for alternative therapies and thus offered very little hope for caffeine, vitamin C, exercise, omega-3, forskolin, co-enzyme Q10, acupuncture or ginkgo biloba, which is thought to be protective for ganglion cells.
Glaucoma management challenges
Dr Ben LaHood looked at glaucoma and cataract and whether cataract surgery should be a standard treatment for glaucoma. Cataract surgery can give an IOP reduction of around 1-3mmHg in those with open angles, though this is more likely in patients with healthy eyes as results can be unpredictable. In stable glaucoma, for patients on medication, if cataract is present it is reasonable to operate, he said, but those with pseudoexfoliation and shallow anterior chambers will receive the most benefit. In poorly-controlled glaucoma, cataract surgery is unlikely to be enough, but MIGS techniques are a great option, he added.
Greenlane clinical centre consultant Dr Chi-Ying Chou discussed the systemic interactions of common medications. Due to nasolacrimal drainage, glaucoma eye drops reach serum concentrations high enough to exhibit systemic side effects and potentially interact with other drugs. This is particularly relevant for the elderly who have low body mass, low body water levels and reduced drug clearance. Children are another at-risk group with high systemic absorption and immature digestive systems. Systemic adverse effects range from bradycardia in amiodarone use to bone marrow suppression after topical chloramphenicol use. Dr Chou urged practitioners to reduce risk by using lower concentrations and showing patients how to perform lacrimal occlusion and consider other treatment routes, and to take extra care when prescribing for the elderly.
Associate Professor Jennifer Craig presented findings from the recent Tear Film and Ocular Surface DEWS II report on ocular surface disease and glaucoma. Patients on topical glaucoma medications are twice as likely to report symptoms of dry eye than those prescribed non-preserved drops. In addition to preservatives, the frequency of drops instillation, duration of treatment and severity of glaucoma also plays a role, she said.
Dr Narme Deva ended this session by reviewing cases studies investigating Avastin and glaucoma, stressing that special care needs to be taken of patients who receive regular intravitreal injections.
Glaucoma case studies
After a nutritious omega-3 rich lunch, delegates were able to take a peep at the latest and greatest instrumentation and products in the trade fair before settling back in for the afternoon sessions. Chaired by Professor Helen Danesh-Meyer, these interactive and entertaining sessions shared real glaucoma case studies from optometrists and ophthalmologists, including Tauranga registrar Dr Keli Matheos, Dr Shenton Chew and some rapid-fire cases from Prof Danesh-Meyer herself. There was much thought-provoking discussion, especially around surgical interventions, which made for a fascinating learning experience.
To end the day, Hilary Goh, a final-year medical student at Auckland University presented her research, which aims to identify nailfold capillaroscopy (NFC) abnormalities in primary open angle glaucoma (POAG) to determine whether NFC can accurately predict the risk of progression.
Glaucoma New Zealand really turned it on this year with education, variety and interactivity. I am sure I am not the only one looking forward to next year’s event.
Ella Ewens is a therapeutically-qualified optometrist at Greenlane Clinical Centre, specializing in CLs, therapeutics and glaucoma.