Immune response contributes to glaucoma?
Immune cells that developed in the eye in response to early exposure to bacteria are a key contributor to progressive vision loss from glaucoma, a research team from Massachusetts Eye and Ear and MIT says. Study findings, published online in Nature Communications, suggest that high pressure in the eye leads to vision loss by setting into motion an autoimmune response that attacks the neurons in the eye — similar to immune responses triggered by bacterial infections. The discovery of these immune cells also reveals a promising new target for future therapies to be developed for the blinding condition.
“Our work shows that there is hope for finding a cure for glaucoma, or even preventing its development entirely, if we can find a way to target this pathway,” said co-senior author Dr Dong Feng Chen, a vision scientist at Massachusetts Eye and Ear and associate professor of ophthalmology at Harvard Medical School. “Current glaucoma therapies are designed solely to lower eye pressure; however, we’ve known that, even when patients with glaucoma are treated and their eye pressure returns to normal, they can still go on to have vision loss. Now, we know that stress from high eye pressure can initiate an immune response that triggers T cells to attack neurons in the eye.”
These findings shed light on a process that largely has remained a mystery ― until now. Glaucoma is a group of eye conditions that often culminate in irreparable damage to the optic nerve, which transmits visual information from the eye to the brain. Elevated eye pressure is known to be the most important risk factor for glaucoma, however, little was understood about how and why patients with high eye pressure go on to develop permanent vision loss. Some patients with glaucoma also do not have elevated eye pressure, and some patients still experience optic nerve degeneration and subsequent vision loss even when their eye pressure is under control.
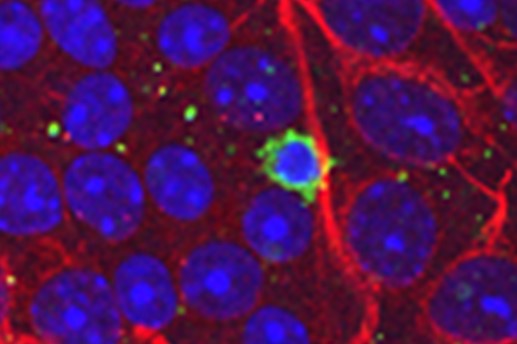
The authors of the study said a newly-observed mechanism explained the series of events leading to permanent vision loss from glaucoma. When pressure in the eye rises, it induces the expression of heat shock proteins, a family of proteins that develop in response to stressful conditions. This leads to a response from immune cells — memory T cells — that are programmed to respond to heat shock proteins. The memory T cells attack the neurons of the retina, leading to degeneration of the optic nerve and often permanent loss of vision. T cell responses are essential in the development of progressive vision loss following elevated eye pressure.
The team studied three groups of mice with glaucoma — some without T cells, some without B cells, and some without T or B cells. Overwhelmingly, they observed a loss of neurons in the mice only if the mice contained functional T cells. More strikingly, development of glaucoma-inducing T cells required early exposure to bacteria; mice never exposed to bacteria (being raised in a “germ-free” facility) were free from glaucoma under elevated eye pressure.
The researchers also studied blood samples from patients with primary open angle glaucoma (POAG), the most common type of glaucoma. In humans, they observed T cells responses similar to the mice that were well over 5-fold higher in patients with POAG compared to samples from patients without POAG.
These findings open the door for the possibility of targeting T cells in the eye as a treatment to halt the progression of vision loss in glaucoma. Heat shock proteins have also been found in other conditions of the eye and the brain, which suggests that these findings could extend to other neurodegenerative conditions as well.