International updates to home-grown problems
The Eye Doctors’ last Grand Round of the year was a good-natured and warm affair. Guests were welcomed by the full Eye Doctors’ team and a choice of refreshments. Zeiss’ Chris Money kicked off proceedings by introducing Zeiss’ new ultra-widefield imaging system, the Clarus 500, said to be the first fundus camera to combine true colour and high clarity with an ultra-wide view of the retina.
Brand new to the market, Money explained why true colour was an important feature of the new technology as it allowed a natural view for better diagnosis. Money also discussed SITA Faster, Zeiss’ newest addition to the SITA family of testing strategies for the Humphrey Field Analyzer 3 (HFA3) perimeter. SITA Faster testing takes about two-thirds of the time required by SITA Fast and about half the time required by SITA Standard, he said, with no blind spot or false negatives.
Xen and the art of trabeculectomy
The evening proper got underway with Dr Mark Donaldson sharing his journey with trabeculectomy surgery and the reticence surgeons have towards applying it given the risks and recovery time, despite its positive effect for many glaucoma patients, especially when micro-invasive glaucoma surgery (MIGS) is not suitable. All eye health practitioners should be mindful of the recovery time and the assistance patients require after surgery given the resultant temporary vision loss, he said, citing one patient who had arranged to stay with relatives for five weeks following surgery, but found it actually took three months before he could manage without outside care.
Thus, Dr Donaldson said he was pleased to discuss a new way of doing trabeculectomy that’s much faster, less-invasive and enables a far quicker recovery, and is now available in New Zealand. The new Xen Implant from Allergan will, he suspected, become a common option for glaucoma patients, whose condition is not being well managed with drops. However, he warned, Xen trabeculectomies have a similar complication profile to trabeculectomy and great care is still required. According to Allergan’s studies, approximately three Xen procedures can be done in the time required for one trabeculectomy, with less intensive and time-consuming follow-up required.
For more on Xen and the new Clarus 500 see December’s NZ Optics.
Retinal cotton wool to RANZCO’s best bits
Dr Andrew Riley took the audience on a rapid tour of retinal cotton wool spots: what causes them, how long they last, what to worry about and what not to worry about.
Cotton-wool spots are small white areas on the retina and are caused by a lack of blood flow to the nerve fibre layer. They usually disappear within several weeks and don’t threaten vision, however, they can be an early sign of diabetic or hypertensive retinopathy and, less commonly, vasculitis, such as the presented case of syphilis. He also discussed the commonest cause of retinal cotton wool spots and reiterated the benefits of Eylea, especially for diabetic retinopathy, which, frustratingly, he said, is still not funded in New Zealand though it is currently being reviewed, again. “90% of patients respond to Avastin, but some patients don’t, so Eylea would be an excellent second line agent.”
One product that is now funded in New Zealand for diabetic macular oedema (DMO), and was proudly on display at RANZCO’s Scientific Congress in Perth at the end of last year, is Ozurdex - a long-acting intravitral steroid, delivered vis a sustained-release ocular implant. Eye Doctors’ Dr Donaldson and Dr Riley were part of the Phase III trial of Ozurdex in DMO and vein occlusions. (For more see December’s NZ Optics.)
Another RANZCO highlight was Alcon’s Ngenuity 3D Visualization System, a platform for digitally-assisted vitreoretinal surgery (DAVS), designed to enhance visualization of the back of the eye, with a variety of colour-enhanced filters. One of the main benefits of this system, however, is the reduction of neck strain for eye care professionals, 50% of which report neck pain due to their posture in surgery and on the slit lamp. “The ‘ophthalmic surgeon stoop’ may become a thing of the past if this could also be included in the slit lamp,” said Dr Riley.
He then closed with some other RANZCO highlights and a comment on defining macular degeneration. “Hard drusen is aging; soft drusen is ARMD.”
Thyroid disease
Dr Shuan Dai gave a memorable, case-based presentation on thyroid eye disease’s diagnosis and management. It can be sight-threatening and debilitating due to its effect on the optic nerve, ocular surface and ocular motility. Non-surgical management includes normalising the endocrine imbalance, stopping smoking, prismatic correction of vertical or horizontal deviation and observation for stability.
It’s important to set appropriate expectations, said Dr Dai, as 20% of cases require more than one surgery; patients may require lid surgery and optic prisms to achieve binocular single vision (BSV); and patients are likely to still have some diplopia in some directions of gaze. The cessation of smoking is very important to maintain long-term stability after successful eye muscle surgery, he stressed.
OSA and floppy eyelids
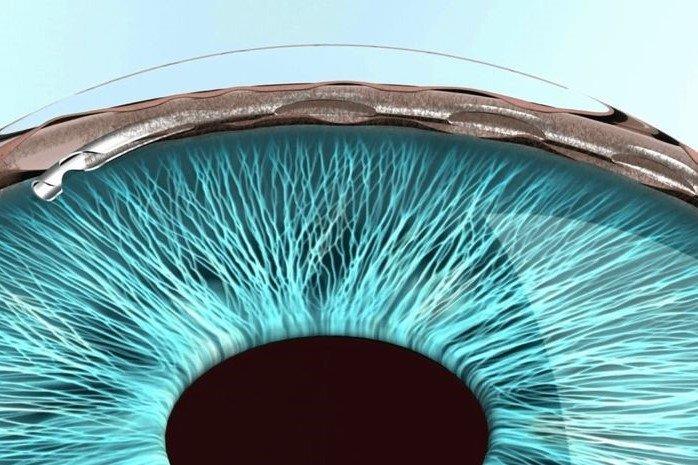
Dr Penny McAllum then discussed her typical corneal transplant patient from South Auckland: a 30-year-old male, usually of Polynesian or Indian descent, with advanced keratoconus, allergic eye disease, floppy eyelids, obesity, obstructive sleep apnoea and, sometimes, diabetes. Using case studies, she discussed the dangers of obstructive sleep apnoea (OSA) and its relation to eye disease, especially keratoconus. OSA patients tend to have red, irritable eyes, and there’s a clear link to allergic conjunctivitis and/or eyelid eczema. 10-20% of patients with OSA have floppy eyelid syndrome (FES) but 96% of patients with FES have OSA. The best ways to manage FES is lubrication at night, tape or shielding eyes at night, treating other eye diseases, such as allergic conjunctivitis, and, when necessary, surgery to reduce horizontal lid laxity, but this has a 25% to 50% failure rate at two years, she said.
OSA is also associated with normal tension glaucoma (NTG), with 5-10% of patients with OSA having NTG, while up to 50% patients with NTG have OSA; more if they also have FES. So treating OSA may stop the progression of NTG, said Dr McAllum.
If your patient has symptoms of OSA, encourage them to talk to their GP about having a sleep assessment, and encourage them to lose weight as this could help save their lives, she added.

Gary Filer, Dr Andrew Riley and Rob Allen

Stephen Hill and Carolyn Campbell