Merging Auckland ophthalmology
A new full-time regional coordinator is being sought to work out how best to merge Auckland’s ophthalmology services to remove disparities of care.
The merger of ophthalmology services across the three Auckland district health boards (DHBs), Counties Manukau, Auckland and Waitematā, has been discussed for many years, but was put on hold last year after the previous part-time regional coordinator left, said Dr Sarah Welch, Auckland DHB’s clinical director. “We would love for it to be expedited. It is a little bit frustrating it’s taken so many years because there is significant disparity across Auckland to the detriment of patients who live in South Auckland.”
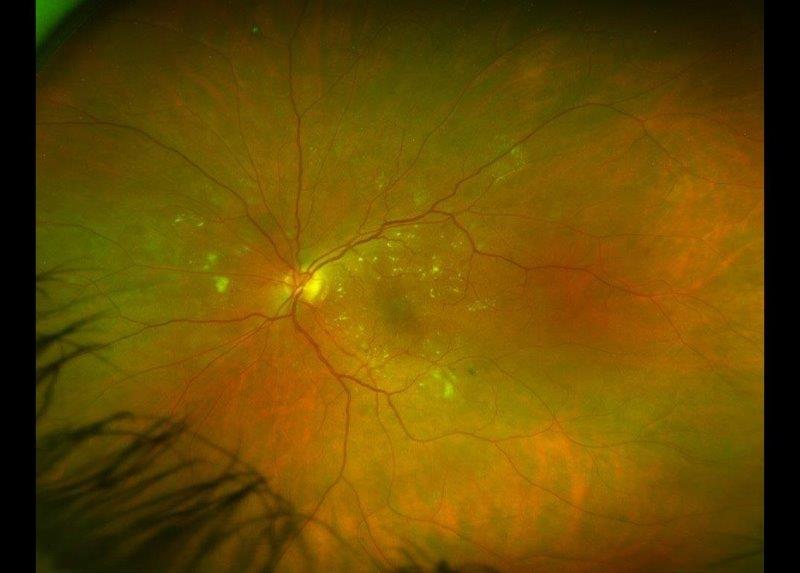
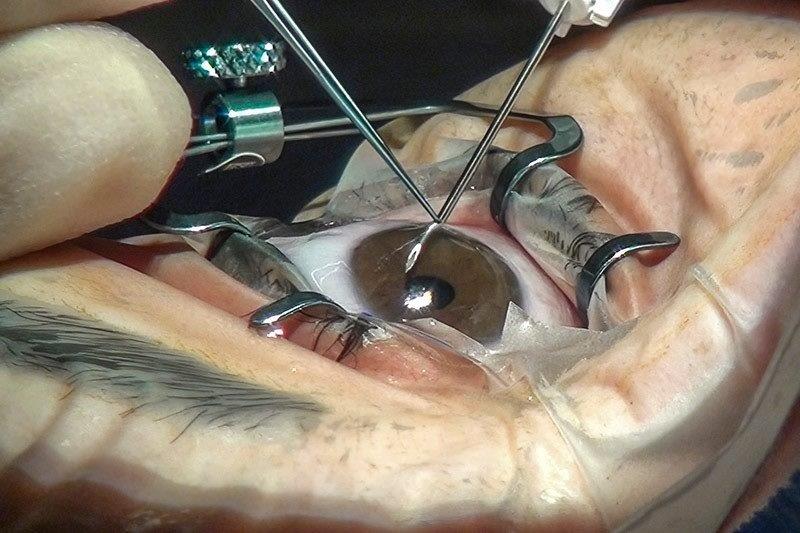
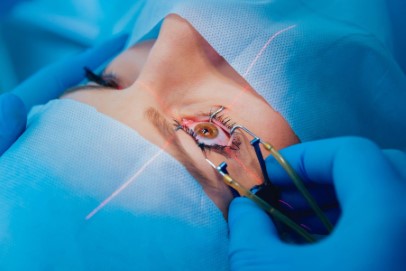
Auckland’s media-dubbed “postcode care” issue, relating primarily to the difference in CPAC (clinical priority assessment criteria) cataract scoring in the region, has been widely documented and criticised, as many South Aucklanders are unable to have cataract surgery until they lose their driving licences. But a merger of ophthalmology services should allow for the better distribution of workloads and specialist staff across the region, said Dr Peter Hadden, Auckland ophthalmologist and chair of the New Zealand branch of the Royal Australia and New Zealand College of Ophthalmologists (RANZCO). “We hope that it will reduce inequity of access to eye health care. However, even in the merged WDHB and ADHB system there are some inequalities, for instance the cataract CPAC score, so we don’t expect everything will be exactly the same for all patients given the current DHB structure.”
The current DHB structure is the main problem, said Dr Welch. “It drives separation, whereas clinical staff want more togetherness. So, the aim of the new regional coordinator will be to work out how we can make the merged ophthalmology structure circumvent the DHB separate structures, so we can work more closely together across the region.”
Doing things differently across the country’s DHBS, such as merging Auckland’s ophthalmology services, to provide better care equity has also been given greater emphasis by the government following the publication of its interim review into the health service published in September last year. Though New Zealand’s health service delivery and per capita costs are in line with other OECD countries, the current system was described as fragmented, overly complicated and lacking leadership.
Chaired by Heather Simpson, the national health and disability review’s interim report also criticised the lack of collaboration in the sector. It didn’t make any recommendations, but it did raise questions it was looking at, including whether it would be better to have fewer DHBs, different functions for DHBs and more sharing of resources across the country.
“The focus must be on the consumer, and what consumers value and need most, with more choice about how needs are met,” said Simpson when the interim report was published. “If future demand is to be manageable, the emphasis must be on preventing ill health and promoting wellbeing.”
A further report is due within the next month.
Dr Welch said she hoped to announce the appointment of a new regional coordinator for Auckland’s ophthalmology services within the next two months. “I would definitely hope we would see a more regional plan by next year and possibly by even the end of this year. That’s my goal!”