Nurses: understanding low vision life
This year’s Ophthalmic Nurses Group meeting was held at the Hilton Auckland alongside The New Zealand branch of RANZCO and the orthoptist’s meeting. There was no conference theme as such, but the conference organisers did themselves proud as speakers covered a diverse range of topics, reflecting their own particular interests, catering to varied interests.
Conference organiser Sue Raynel, research programme manager at the University of Auckland, couldn’t be there to see her efforts come to fruition as she was visiting Janet Marsden, a well-known and respected ophthalmic nursing colleague from the UK who was sadly in the last stages of terminal cancer (see obituary, this page). Janet had been influential in the development of advanced ophthalmic nursing practice around the world and we as a profession owe such a lot to her. She had been a regular guest speaker at the Ophthalmic Nurse Group meetings here in New Zealand and we gained much from her wealth of experience and her vision for the role nurses can play in improving the patient’s journey. Her strong presence will be very much missed.
The guest speaker for this year’s nurses meeting, Helen Gibbons, is the lead nurse for education and research at Moorfields Eye Hospital in London. Her talk on visual awareness encouraged us, as clinicians, to walk in the footprints of the sight-impaired. Helen discussed how she and her fellow ophthalmic nurses, during training, wear special blindfolds and take to the streets, try to cook a simple meal or manage other simple household chores, or just sit in the waiting room at Moorfields, listening to instructions they have no idea how to follow, to give them a glimpse into the lives of their patients. Stories of spaghetti sauce being splattered across kitchen walls highlighted the struggles patients have to face every day with fading vision. Helen emphasised vigilance to conference attendees when working in the clinic environment, to not just call out to patients and disappear into clinic rooms expecting them to see where you have gone. It is important not to forget we are managing patients who are in some cases significantly vision impaired, requiring physical guidance within the eye clinic environment.
Helen also shared her experiences as a research nurse and the advanced nursing roles at Moorfields Eye Hospital which, I’m sure, left many of us inspired to take on more skills and responsibilities to improve efficiency and continuity in patient care. For example, nurses undertaking YAG laser capsulotomies.
Helen also discussed an orientation programme Moorfields has developed for nurses new to ophthalmology. This provided many new ideas about how to orientate new staff members into our ophthalmic environments. Lastly, Helen shared one of her passions with us, a large project to set up an eye clinic in Africa, which seemed very challenging but clearly, hugely rewarding.
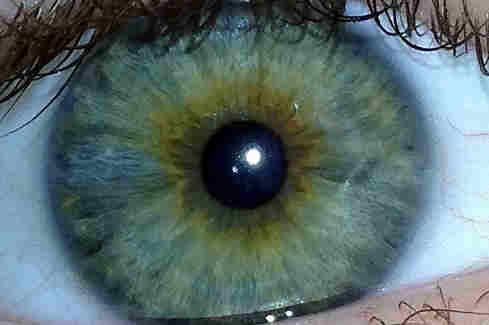
The rest of the nurses meeting programme was filled with familiar faces behind the podium, all happy to share their skills and knowledge. Auckland District Health Board clinical nurse specialist, Olga Brochner, injected her usual humour into her talks… “Vitreous is like a teenager, it just blobs around and occasionally causes trouble!” Along with Auckland ophthalmologist David Squirrel, she also presented a very humorous Kiwi interpretation of optical coherence tomography (OCT) which was “Sweet as”! OCT has become such a valuable tool in diagnosing and monitoring macular disease: the knowledge gained from this talk was not only useful for the workplace but also in understanding subsequent presentations involving the retina, such as those relating to macular oedema and diabetic retinopathy.
It was also interesting to hear about new developments around the country where eye clinics are managing the huge workloads by extending nurses’ skills and collaborating with optometrists in glaucoma monitoring, for example, as Jane Hawthorne from Hawkes Bay explained. In Rotorua nurses are undertaking cross linking, while nurse-led clinics are catering to increasing demands in the Hutt Valley, Waitakere (for glaucoma) and Auckland, where there’s now a gateway clinic to manage diabetic retinopathy.
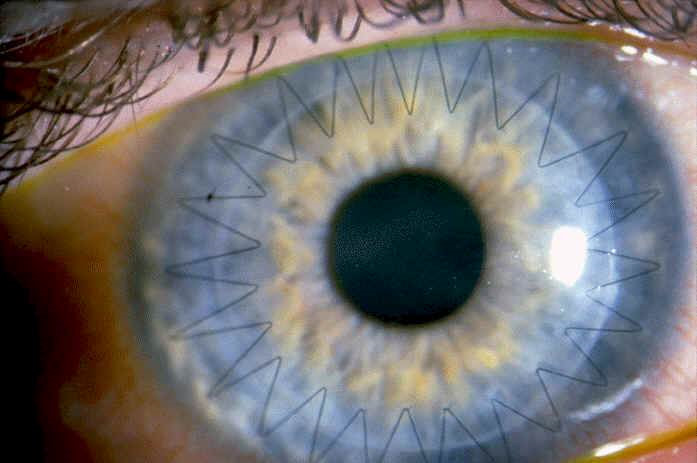
There were several interesting case studies presented by nurses, including latanoprost causing macular oedema, STIs, hydroxychloroquine and telescopic lenses for AMD. Our medical colleagues also presented updates on dry eye, the corneal bank, macular degeneration, corneal grafting and the New Zealand cataract risk stratification, to name but a few. While other RANZCO guest speakers shared recent study results from stem cells treatments for retinitis pigmentosa, Stargardt's disease, and AMD, and discussed how to increase the effectiveness of current medications now available now for uveitis and macular degeneration.
Overall it was a well-run conference and, on my first day back at work following the conference, I found I was drawing upon the education I had gained in managing my patients, which is why attending conferences such as these is so valuable.
About the author
Fiona Bamforth is an ophthalmology clinical nurse specialist based in Northland