Orthoptists: crossing ophthalmology divides
New Zealand’s Orthoptic Society annual conference, held in parallel with the RANZCO NZ Branch meeting in Auckland, proved to be another interesting event and discussion between ophthalmology professions, both from the selection of speakers and among orthoptists after the sessions.
Genetics and quackery
In the opening cross-conference keynote sessions, Professor David Mackey and Dr Brendon Vote shared some of the amazing inroads genetic research is making both in disease classification and possible new treatment techniques. Prof Mackey also highlighted that in this era of ‘Dr Google’, we need to help teach our patients, who might be thinking in desperation of enrolling in new drug trials, how to recognise a quality trial from quackery. The former shouldn’t require upfront fees; should have ethical approved and should be run by organisations which do quality research. Patient organisations and charities, such as Macular Degeneration NZ, can help steer patients in the right direction, he said.
This was followed later in the programme by Dr Juliet Taylor who presented a brilliant and thorough clinical genetics talk that helped elucidate the complicated topic of our rare syndromic children, reinforcing the critical observation and pattern recognition skills we have that help us to put the jigsaw pieces together to make a correct diagnosis.
Neuro-ophthalmology
Dr Jesse Gale opened the sessions on neuro-ophthalmology providing a great number of pearls about reviewing CT and MRI scans, and why the image choices, T1, T2 and gadolinium contrast, are chosen, and finishing with some interesting cases highlighting the differences. In summary:
- CT is best for blood vessels and calcium deposits and metal FB
- MRI can pick up calcium deposits (dark) but is best to pick up water and how it interacts with the brain. T1 - grey matter is great and white matter white; T2 opposite
- Flare with T1 removes the water image so that inflammation shows up
- T1 with gadolinium reveals orbital lesions or inflammation plus fat
- PET scans are a type of CT, but with specific disease markers can help us see how the disease is interacting with the body
Ocular myasthenia gravis
Dr Taras Papchenko gave a really interesting presentation on myasthenia gravis (MG), an autoimmune disease that affects the neuro-muscular junction resulting in classical symptoms of variable muscle weakness and fatigue, and current theories about why the eye muscles are affected first. I particularly liked the update that up to half of ocular MG patients may not respond with acetylcholinesterase inhibitors, especially those with diplopia, but prednisolone has been shown to have a favorable response. It is less common in those in the first decade of life and over 70, is more common in men, with non-ocular MG being more prevalent in women, and 30% can have anti-thyroid antibodies. All patients with suspected or known MG need a chest CT to look for thymic hyperplasia or thymoma.
Orthoptist Rachael Grierson’s presented a case on juvenile ocular MG, prompting a good discussion about this rare condition. The discussion on this topic continued following my talk about a male patient with recurrent nerve palsy and a neurological diagnosis of ocular migraine, with agreement that in such cases ocular MG should also be considered.
Nystagmus, Squint Club and aniseikonia
Dr Stuart Carroll gave a fun and useful talk on ocular motor apraxia and periodic alternating nystagmus, with the proviso to watch for a few minutes to see if direction changes. Nystagmus can occur from ocular albinism or cerebellar insult, he said, reminding us (through some great nystagmus videos) as well about Alexander's law in vestibular lesions, where nystagmus amplitude increases in the position of gaze, corresponding to the jerk direction in a vestibular lesion.
Those orthoptists who were lucky enough to receive funding to attend this year’s Squint Club meeting in Melbourne provided feedback from the best talks. This included new information and background on ‘saggy eye syndrome’ or (the politically correct term) ARDET; age-related distance esotropia; and news about an exciting new drug (teprotumumab) for thyroid eye disease, currently in phase II trials, which is showing promising results. For more about this year’s Squint Club meeting, see http://www.eyeonoptics.co.nz/articles/archive/squint-club-2018/
Dovetailing with the squint club meeting, Tammy Miller presented an esotropia case providing a good reminder about the optical enhancement that occurs in high refractive index glasses, while Jay South presented research from her masters on whether image size matters in anisometropia. There is natural unaided aniseikonia caused by the axial length and structure of the eye before you add on the spectacle element too, she said. The protocol is to fully correct the anisometropia, but the total level of aniseikonia (image size c, glasses-image size s gls) may put it over the 5% disabled limit. We can treat this optically with special aniseikonic lenses (such as Shaw) but we cannot treat anatomical aniseikonia. Contact lenses can help with correcting induced-aniseikonia, but should we consider Rx for amblyopia? A question for the future as Shaw lenses are very expensive and not cosmetically appealing.
Low vision updates and other highlights
Blind Foundation orthoptist Claire Fitzgerald updated us and sought feedback about the foundation’s future direction. This included electronic referrals for non-specialist practitioners; functional vision assessment options for registration criteria rather than the current acuity and visual field grading; and more orthoptists working in low vision therapy in New Zealand similar to the Australian system, to allow for improved access to services. Currently there are just two orthoptists in this role in Wellington and Dunedin, and they are both part-time.
Sticking to the low vision theme, keynote nurse speaker, Helen Gibbons from Moorfields in London, shared her organisation’s Visual Awareness Training, re-confirming that all of us are here to make life better for our patients and that being empathic to their situations is a key part of our assessments. The simple act of walking with patients from the consulting room, rather than just calling their name in a busy waiting room relieves stress and thus improves assessment quality. This visual awareness training is something I am going to bring back to add to our own in-house professional development for new nursing and technical staff.
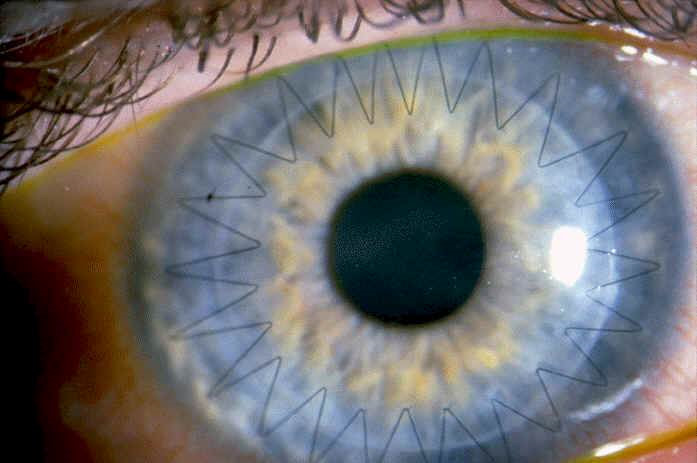
Dr Malisa Ami gave an interesting presentation about congenital syphilis, a disease that is being seen more frequently and we need to consider as it’s classed as a ‘great masquerader’. Inflammation is very common and it is still a highly treatable disease when caught early. Another highlight for me was Jo Kennaway’s case of a three-year-old who presented with an esotropia and motor developmental delay. Fundi examination showed pale optic disc LE and temporal OD pallor of the right eye; there was no previous history of NF1 and the child did not meet clinical grading, but on examining the mother she met the clinical diagnosis, which then meant the child met the threshold. This case highlighted the fact that we need to be vigilant on routine strabismus referrals. While Mij McPhie shared an interesting case on occlusive IOL implant and removal, highlighting how picking an opaque IOL allows OCT transparency to check the retina.
Orthoptic Society business
We concluded the meeting with our AGM and the election of new officers: Nia Stonex has been elected to president replacing Carly Henley who had finished her term (grateful thanks were given to Carly for all her work for the society); Noirin Kiely is vice president; Libby Kelly will finish her term as secretary in 2019; while Tammy Miller has agreed to stay on for a second term as treasurer and website producer. I will remain as Allied Health Association of New Zealand representative until 2019 and Mij McPhie is happy to continue running the online journal review rota.
About the author
Orthoptist Sally-Anne Herring is a regional specialist in eye movement disorders and their treatment from Hawke’s Bay to Gisborne and former secretary of the New Zealand Orthoptic Society.