RVO, MIGS, red eye and more
Optometrists from all parts of the South Island attended the ever-popular annual Christchurch Eye Surgery Study Day on the 14 March 2020. Christchurch Eye Surgery is a purpose-built facility developed in collaboration with nine local ophthalmologists, who come together every year to deliver a series of comprehensive lectures in one full-day’s programme.
Given it occurred before lockdown but under the shadow of Covid-19, this year’s study day was only made possible by the work of a dedicated team who prepared everything from readily available hand sanitisers to pouches of tissues distributed to delegates. This team of friendly faces, Natasha, Sarah-Jane, Margaret, Rachel and Careen, are all staff from the surgery.
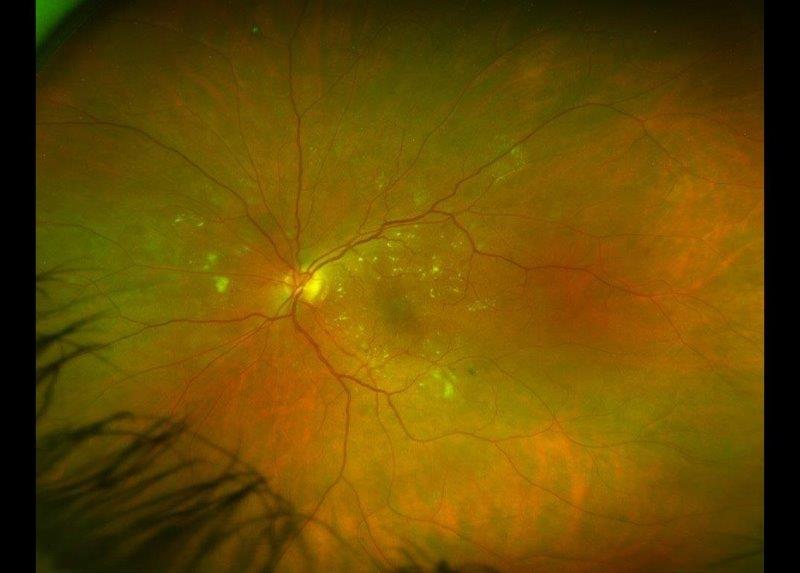
The morning’s programme began with Dr Sean Every’s topic of retinal vein occlusion. He described the successes and limitations of diagnostic tests, like fluorescein angiography, and of treatments when associated with macula oedema. He recalled how macula-grid laser photocoagulation was the mainstay treatment for non-ischaemic macula oedema following BRVO in the early 2000s, but now it has been superseded by anti-VEGF treatment, like Avastin, Lucentis and Eylea injections.
Dr Ian Dallison presented a personal account of six months’ experience with minimally invasive glaucoma surgery (MIGS), which was showing promising results in a group of his patients with uncontrolled glaucoma who would normally have needed trabeculectomy. MIGS devices focused on lowering intraocular pressure (IOP) and had high safety profiles, with rapid recovery rates. Although some provide only modest IOP reductions, they do reduce drop-dependence for the patient, he explained.
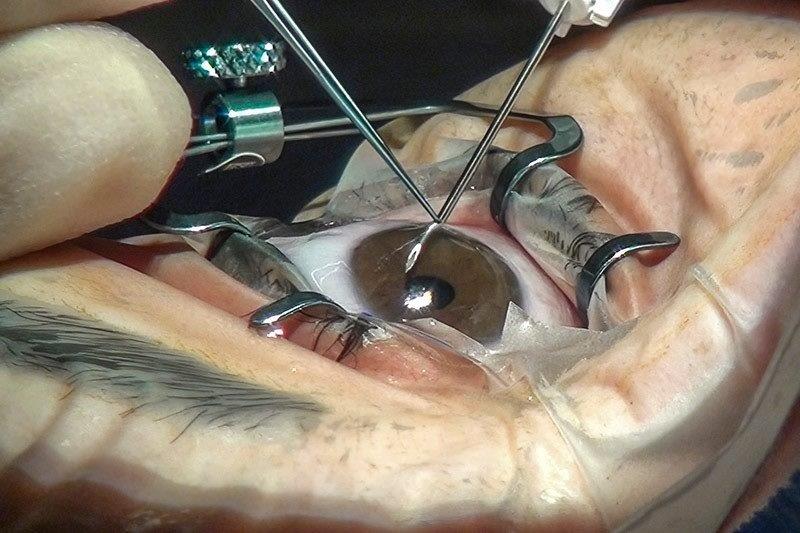
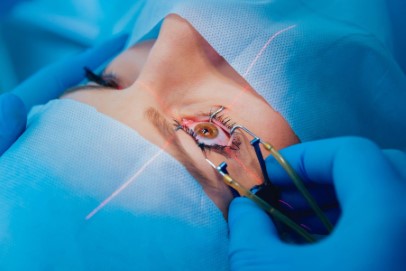
Continuing the subject of minimally invasive surgeries, Dr David Kent described small incision lenticule extraction (SMILE) for refractive surgery as comparable to femtosecond laser-assisted in situ keratomileusis (FS-LASIK) in terms of safety and efficacy. Moreover, it has the advantages of better ocular surface stability and bio-mechanical strength, when compared to FS-LASIK, he said. He emphasised the importance of patient selection, in alignment with the US Food and Drug Administration-approved guidelines, and the use of nomogram to enhance the predictability of SMILE. His five-minute real-time surgery video reminded us all of the incredible accuracy of laser incisions.
Responding to last year’s conference feedback, Dr Malcolm McKellar then guided us through a myriad of red eye presentations and set us on a better path of diagnosis and management. He offered a range of red eye diagnoses as diverse as his descriptive language from “violaceous hue” to describe a case of scleritis to cautioning us with the phrase “beware of the white eye”.
With the title Do carrots really help us to see in the dark?, Dr Rebecca Stack’s talk stirred our curiosity into the role vitamins and supplements play in eye diseases. The presentation was a glorious pharmaceutical sampling of uses and contraindications of compounds, from the well-known vitamin A, omega 3 and zinc to the forgotten, arsenic and silver, and the undoubtedly now fashionable, cannabis.
Dr Jo-Anne Pon presented information from landmark studies into the most common forms of optic neuropathy. The optic neuritis treatment trial (ONTT) did a wonderful job of providing guidance to treat typical cases of optic neuritis, she said. Dr Pon also discussed the treatment successes and failures of nonarteritic anterior ischemic optic neuropathy (NAION) and idiopathic intracranial hypertension (IIH), giving us a strong appreciation of the amount of time she’s had to devote to wading through clinical trials and journals.
Dr Logan Robinson then provided a detailed interpretation of macula optical coherence tomography (OCT) scans, showing us how to find meanings in these mesmerising green, yellow and red images. While new team member, Dr Liz Conner discussed herpes and the eye, sharing some clinical pearls about this “creeping eye problem” and quoting references from the Herpetic Eye Disease Study II and Herpes Simplex Virus Keratitis: A Treatment Guideline 2014.
The Study Day concluded with a recollection of the changes in ophthalmology over the past 35 years by Dr Jim Borthwick. He remarked on cornerstone surgical practices like phacoemulsification cataract surgery and anti-VEGF treatments, as well as advances in diagnostic tools that were a godsend for both optometric and ophthalmic clinicians. For example, the widespread use of double aspheric lenses for indirect ophthalmoscopy, introduced in the ‘80s, or the arrival of OCT to achieve in-vivo human retinal images in the late ‘90s.
Dr Borthwick even managed to source a nostalgic selection of photographs from old hospital buildings to the luminaries of Christchurch ophthalmology over the years. He recalled the standing joke among hospital staff in the 1990s about the department: “The eye department on the top floor of the hospital building commands the best view of the city, yet they always have their black curtains permanently drawn.”
This year’s study day also provided us with the opportunity to review some of our clinical understandings and delve into tricky areas in the popular Ask an expert panel session at the end.
The whole day flew by quickly as we connected with colleagues and remained somewhat on edge discussing the developing Covid-19 situation. Most delegates predicted this conference day would probably be our last educational meeting for the year. I surely hope not.
Therapeutic optometrist Theresa Slaten began her career with Dunedin Hospital before joining OPSM just before the Christchurch earthquake. She currently works in the southern-most city of New Zealand, Invercargill.