Scleral lens fitting for high levels of regular astigmatism
In my February 2016 column, I described how mild to moderate levels of regular astigmatism can now be corrected with orthokeratology. However, for some patients the lifestyle consideration of using ortho-K lenses may not suit, or they may just have too much astigmatism to realistically be a good ortho-K candidate. Hopefully most optometrists will know a rigid lens is the best option for these >3.00DC patients to achieve high quality vision. For the majority of patients an RGP corneal lens will work fine, however for patients desiring comfortable all-day wear and stable vision a larger scleral lens can be a preferable option in many instances.
In this example my patient, a 25-year-old male, reported to our practice to investigate his contact lens options. He is a university student in the health area and plays basketball at a representative level. Unfortunately, he has high amounts of astigmatism (R +5.50/-4.50 x 168, L +5.25/-4.25 x 11, 6/5 in each eye) and came to his appointment wearing glasses, which he was very happy with. He had tried several different contact lens options in the past with little success; Customised soft toric disposable lenses had good comfort but the vision was poor and fluctuated. Rigid gas permeable bi-toric corneal lenses were tried but were poorly tolerated due to comfort despite providing good vision. They had also popped out twice during basketball games. Discouraged by this our young patient got the opinion of a corneal specialist who told him a clear lens extraction was the only permanent opinion. After discussion of his options we decided to fit a toric periphery scleral lens to be used when the patient needed to be without his spectacles.
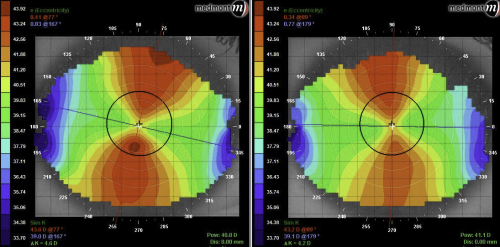
Corneal topographies in Medmont Studio showing the regular limbus-to-limbus WTR astigmatism
Until scleral mapping with technology such as the Eye Surface Profiler (Eaglet Eye) becomes commonplace in contact lens practices, trial fitting scleral lenses is still required. This can be a problem in this sort of case however, as a rotationally symmetrical trial lenses will rock along the steeper vertical meridian of a high WTR cornea. While the lens is still reasonably comfortable, a rocking lens can allow bubbles under the lens and can increase the likelihood of the patient inadvertently blinking the lens out during the fit. I have made a request that a non-rotationally symmetrical scleral trial set be available in the future for just this instance.
A topography over the EyeSpace Scleral (Innovative Contacts) trial lenses I fitted to this patient showed significant with-the-rule flexure of around 2 diopters after only a few minutes. Over-refraction through the lens at this point also showed -2.00D of residual astigmatism with axis 180.
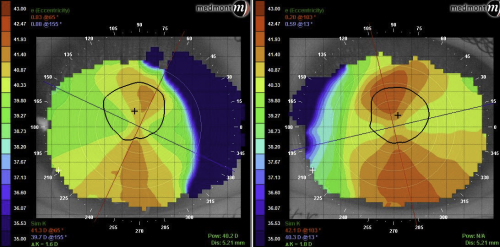
Topography over the rotationally-symmetrical trial lenses shows significant flex on the toric anterior surface
I talked about minimising scleral lens flexure in the October 2015 issue of NZ Optics. It is clear that a rotationally symmetrical lens would continue to rock and cause stability issues in this patient, even with a thicker centre thickness. A lens with a difference in sagittal height in each meridian will stabilise the lens and eliminate flexure much better. The lenses were ordered with 500um difference in sag (to account for ~2.50D of flex) between the meridians.
Following a delivery and teach appointment and some final tweaks to the lens fit during aftercare visits (A more detailed report of this case can be found at eyespace.com.au/blog) the patient returned 2 weeks after picking up his final lenses. He reported vision with his new lenses was excellent and comparable with his glasses. Comfort was also reported to be very good. Vision with each lens was 6/6+2 after 4 hours of wear with no significant residual astigmatism or flexure in the over-topography.
Anterior OCT of these lenses showed the central apical clearance was measuring in the low 200um. This clearance could be further decreased into the 100-150um range if desired with the predictability afforded to us by modern lathe technology.
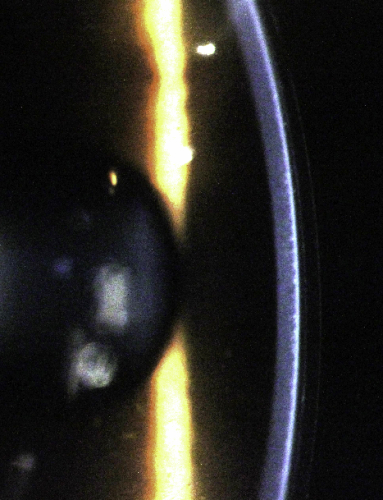

Apical clearance in the new lenses as seen with the slit-lamp and OCT
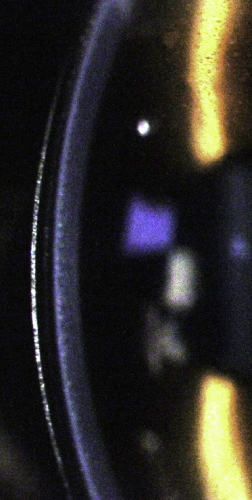
The appearance of the of the lens under the slit-lamp showed very little conjunctival vessel impingement. Upon removal, aside from some mild staining atop small pingueculae in each eye, there is no evidence of lens impression or abrasion. The cornea was also devoid of defect.
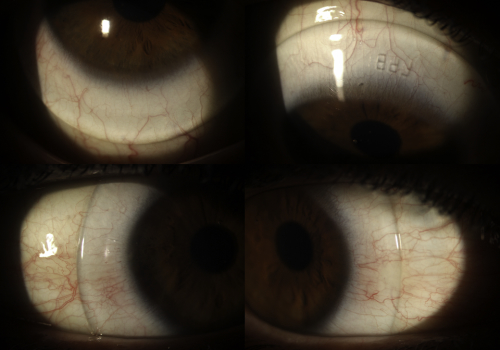

Scleral landing zone profiles of the right lens. Note the lack of conjunctival blanching at the lens edge
Overall the patient was very happy with the outcome of his scleral lens fitting. Careful assessment of the cornea for signs of hypoxia and toxicity is important during his future follow-up visits as the thickness of the lens and tear reservoir can pose barriers for oxygen to pass to the cornea, even with the high Dk materials used in modern scleral fitting. A key concept here is that a toric cornea can achieve great vision in a scleral lens with a spherical back optic zone. The difference in sagittal height of the peripheral areas is important, as this controls stability and flexure on the eye. This case shows that specialty scleral lenses are not just reserved for diseased or compromised corneas but can be a useful and effective tool in treating regular ametropias in practice.
About the author
Alex Petty is a Kiwi optometrist who graduated from the University of Auckland in 2010. He has an interest in specialty contact lenses, ortho-K and silmoparis.com myopia control.



























