Screening of infants for ocular abnormalities
Preventing childhood visual impairment is a priority of the World Health Organisation’s “Vision 2020 - The Right to Sight” due to the high emotional, social and economic cost for the individual and the wider community. Many causes of childhood visual impairment are preventable. Ocular screening programmes for newborns are recommended to ensure timely detection and treatment of common paediatric ocular conditions. All newborns in New Zealand should have their eyes checked with the red reflex test by their lead maternity carer, which may be a midwife, general practitioner or obstetrician1. In addition, specialist retinal screening is available for infants at risk of retinopathy of prematurity, those born extremely premature (<30 weeks gestational age) or infants with a very low birth weight (<1250 grams)2.
Red reflex
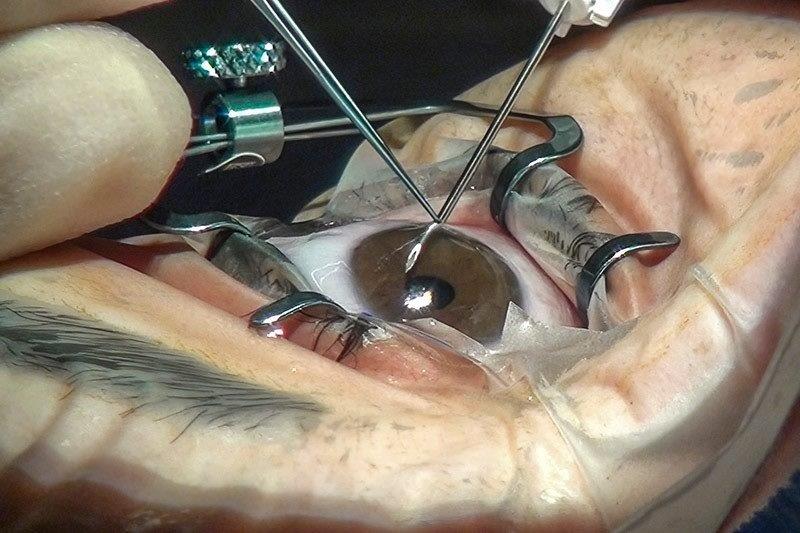
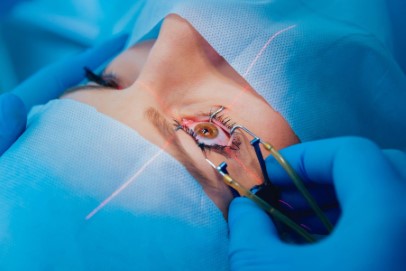
The red reflex test is an essential part of the neonatal assessment in New Zealand with the examination technique and timeline outlined by the New Zealand Government in the Well Child/Tamariki Ora Practitioner's Handbook1. The red reflex test is a simple, non‑invasive and easy to implement screening technique first described by Brückner in 1962, displayed in Fig 13. An abnormal red reflex can indicate sight threatening, life threatening, or systemically associated conditions such as congenital cataracts, retinoblastoma or metabolic disorders3. The ‘red reflex’ is the reflection of the ophthalmoscope light off the fundus, with any impediment in the normally clear ocular media resulting in an abnormal red reflex appearance3. A normal red reflex, is defined by the American Academy of Paediatrics, as equal and symmetric in both eyes, with no dark spots, opacities or white reflexes3. Screening guidelines in New Zealand recommend screening in the first week of life and at six weeks of age by the lead maternity carer, general practitioner or paediatrician1.

Fig 1. Red reflex examination
In New Zealand, for all infants with an abnormal red reflex or a family history of inherited ocular disorders a full ophthalmic examination is recommended1, 3. However, cases of missed newborn ocular pathologies are not uncommon. For example, in the UK where red reflex screening is standard practice, a retrospective review of congenital cataracts by eight weeks of age showed only 47% of cases had been identified4. A clinical audit in Greenlane Clinical Centre, New Zealand’s largest tertiary eye referral centre, showed less than 1 out of 50 congenital cataracts were picked up through red reflex tests performed during the newborn period. This is of great concern as the optimal surgical treatment for congenital cataracts to maximise visual outcomes is four to six weeks of life5. A study of dilated red reflex examinations of 37 paediatric eyes failed to detect all 13 cases of retinoblastoma in an at‑risk group6. Reasons for the reduced detection rate are likely multifactorial, possibly relating to inadequate training, implementation of the red reflex test, and the sensitivity of the test itself.
A 2016 survey of practitioners in Auckland who undertake the red reflex test revealed the red reflex test is not consistently performed in New Zealand, with more than 80% of practitioners reporting they had not received any formal training7.
In New Zealand, up to 20% of lead maternity carers do not perform the red reflex test as the national standard dictates8. Many stated a lack of appropriate training or equipment as the key barrier to providing care8. The sensitivity of the red reflex test is also a factor. A large population study published in Paediatrics in 2016 comparing the red reflex test to a comprehensive eye examination, showed an anterior segment disease sensitivity of 99.6%, but only 4.1% for posterior segment disease9. Therefore, without overcoming logistical, sensitivity, and educational challenges vision impairing ocular opacities and posterior disease may still be missed4.
Retinopathy of prematurity screening
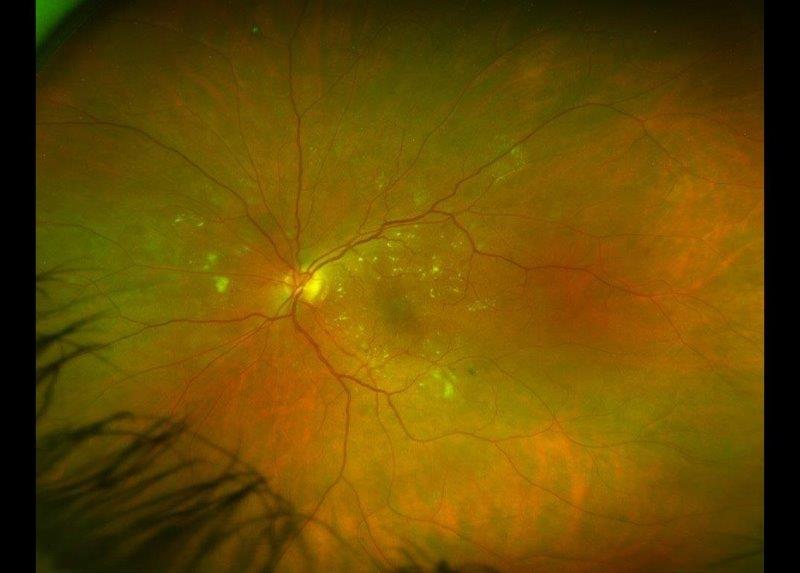
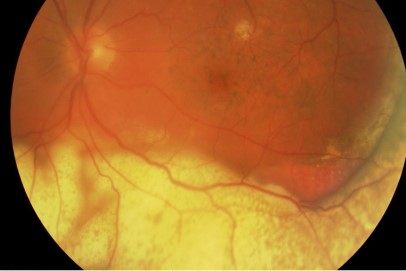
Retinopathy of prematurity (ROP) is a disease affecting low birth weight and extremely premature infants. Screening to detect ROP is recommended for all at‑risk infants by the World Health Organisation. However, worldwide the numbers of infants at risk of ROP is increasing and the number of ophthalmologists willing to screen is decreasing. Reasons for the decreasing number of ophthalmologists in ROP screening include low reimbursement, liability concerns and complex logistic coordination10. The development of wide‑field digital imaging (WFDI) as a potential alternative for ROP screening may alleviate the current workflow challenge. WFDI is a fast, cost-effective and accurate examination approach that has low impact on the infant and results in an objective record11, 12. The introduction of the RetCam has opened the opportunity for telemedicine assessment of images, with ophthalmologists able to remotely assess images captured by trained allied health professionals13. RetCam WFDI can be successfully performed by specialist nurses, allowing ophthalmologists to analyse images at a remote site and a later time14. The options of telemedicine and utilising allied health professionals potentially increases access to ocular assessment in a timely fashion.


Fig 2 & 3. RetCam infant ocular camera and wide-field digital image of a normal infant retina)
The need for timely and accurate ROP screening to detect treatment-warranted ROP has been clearly established. In Auckland, a world‑first screening programme exclusively using WFDI to detect and manage ROP, known as the Auckland Regional Telemedicine ROP network (ART‑ROP) was launched in 2006. ART‑ROP now covers three District Health Boards and four neonatal intensive care units. Appropriate, accurate and regular retinal examinations to detect the presence of treatable ROP have well‑documented clinical benefits. Since the implementation of the ART-ROP telemedicine screening, severe visual impairment from ROP in the greater Auckland region has been reduced to nil from two infants per year in the prior decades15.
It’s important to note that if WFDI is to be used for ROP screening it must be demonstrated it can detect treatment-warranted ROP equivalent or better than binocular indirect ophthalmoscope (BIO) screening. A number of studies in a variety of locations have confirmed that WFDI has a high sensitivity for detecting treatment‑warranted ROP. Comparison of techniques in New Zealand observed 100% sensitivity and 97.9% specificity in detection of treatment requiring ROP12. Telemedicine screening for ROP has also been determined as an accurate diagnostic tool with high inter‑ and intra‑grader reliability13.
The use of non-ophthalmologists for capturing ROP screening images has been shown to be a safe and effective alternative16. In a prospective comparison study of time required by ophthalmologists to perform BIO versus telemedicine diagnosis of ROP, BIO took over four minutes per infant compared to under two minutes with telemedicine17. The objective photographic record produced with WFDI is advantageous with utility for in-medical liability cases, seeking of second opinions or comparing changes over time11.
Screening guidelines for ROP must be specific and determined locally, due to regional variations in neonatal care and survival of extremely premature and low birth weight infants. In New Zealand, all infants born less than 30 weeks gestational age or weighing less than 1250 grams at birth are screened for ROP2. Infants deemed to be at high-risk due to a tumultuous clinical course, as determined by their attending neonatologist are also screened2.
Potential future screening
In addition to ROP screening, WFDI can be utilised for many paediatric ocular conditions. It can be used for documenting retinoblastoma, paediatric glaucoma to assess efficacy of treatment over time. It can also be used for objective documentation in cases of suspected non‑accidental injuries, or for photographing anterior or posterior conditions to seek a second opinion.
The success of ROP WFDI with telemedicine has led to the suggestion of utilising the system for universal newborn eye screening for all newborn ocular abnormalities. WFDI of a cohort of 3573 healthy full‑term newborns in China by Li et al, found abnormal ocular findings in 24.4% of cases, with the majority being retinal haemorrhages18. Other ocular abnormalities included congenital cataract, microphthalmos, retinal hamartoma and optic nerve anomalies18. A similar study was completed by Vinekar et al in India. From the 1021 infants screened, 4.7% had abnormal findings, 52% being retinal haemorrhages19. A prospective universal newborn eye screening study has been undertaken in Auckland with similar findings. Final results will be published shortly. The high number of birth‑related retinal haemorrhages is of interest due to the unknown longer‑term outcomes particularly for those which are long‑standing or obscure the macula. The potential for earlier detection of a range of ocular abnormalities through universal newborn eye screening may offer more timely detection and thus, management of sight or life-threatening abnormalities.
Newborn ocular screening is an important aspect of newborn checks and improvement of current detection rates must be made to give every child the best possible start to life.
References
- Ministry of Health. Well Child/Tamariki Ora Programme Practitioner Handbook: Supporting Families and Whanau to Promote their Child's Health and Development. Wellington: Ministry of Health; 2013.
- Kuschel CA, Dai S. Newborn Services Clinical Guideline - Retinopathy of Prematurity. 2007;2017.
- American Academy of Pediatrics, Section on Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology, American Association of Certified Orthoptists. Red reflex examination in neonates, infants, and children. Pediatrics. 2008;122:1401-1404.
- Rahi JS, Dezateux C. National cross sectional study of detection of congenital and infantile cataract in the United Kingdom: role of childhood screening and surveillance. The BMJ. 1999;318:362-365.
- Lambert SR. Treatment of congenital cataract. Br J Ophthalmol. 2004;88:854-855.
- Khan AO, Al-Mesfer S. Lack of efficacy of dilated screening for retinoblastoma. J Pediatr Ophthalmol Strabismus. 2005;42:205.
- Raoof N, Dai S. Red reflex screening in New Zealand: a large survey of practices and attitudes in the Auckland region. N Z Med J. 2016;129:38-43.
- Fry M, Wilson GA. Scope for improving congenital cataract blindness prevention by screening of infants (red reflex screening) in a New Zealand setting. J Paediatr Child Health. 2005;41:344-346.
- Sun M, Ma A, Li F, et al. Sensitivity and Specificity of Red Reflex Test in Newborn Eye Screening. J Pediatr. 2016;179:192-196. e4.
- Altersitz K, Piechocki M. Survey: physicians being driven away from ROP treatment. Ocular Surgery News. 2006.
- Chiang MF, Melia M, Buffenn AN, et al. Detection of clinically significant retinopathy of prematurity using wide-angle digital retinal photography: a report by the American Academy of Ophthalmology. Ophthalmology. 2012;119:1272-80.
- Dai S, Chow K, Vincent A. Efficacy of wide‐field digital retinal imaging for retinopathy of prematurity screening. Clin Experiment Ophthalmol. 2011;39:23-29.
- Richter GM, Williams SL, Starren J, Flynn JT, Chiang MF. Telemedicine for retinopathy of prematurity diagnosis: evaluation and challenges. Surv Ophthalmol. 2009;54:671-685.
- Shah SP, Wu Z, Iverson S, Dai S. Specialist Nurse Screening for Retinopathy of Prematurity-A Pilot Study. The Asia-Pacific Journal of Ophthalmology. 2013;2:300-304.
- Tan Z, Chong C, Darlow B, Dai S. Visual impairment due to retinopathy of prematurity (ROP) in New Zealand: a 22-year review. Br K Ophthalmol. 2015;99:801-806.
- Shah S, Dai S. Safety of Specialist Nurse Screening for Retinopathy of Prematurity—Response to Letter. The Asia-Pacific Journal of Ophthalmology. 2013;2:420.
- Richter GM, Sun G, Lee TC, et al. Speed of telemedicine vs ophthalmoscopy for retinopathy of prematurity diagnosis. Am J Ophthalmol. 2009;148:136-142. e2.
- Li L, Li N, Zhao J, et al. Findings of perinatal ocular examination performed on 3573, healthy full-term newborns. Br J Ophthalmol. 2013;97:588-591.
- Vinekar A, Govindaraj I, Jayadev C, et al. Universal ocular screening of 1021 term infants using wide‐field digital imaging in a single public hospital in India – a pilot study. Acta Ophthalmol. 2015;93:e372-e376.
About the authors
Samantha Simkin is a therapeutically qualified Optometrist who completed her PhD in the Department of Ophthalmology at the University of Auckland on paediatric visual impairment, where she is now a post-doctoral research fellow.
Dr Shuan Dai is a Consultant Ophthalmologist who specialises in Paediatric Ophthalmology and Adult Strabismus Surgery practicing at Greenlane Clinical Centre and Eye Doctors. He is the clinical lead in Paediatric Ophthalmology and Strabismus at Auckland District Health Board. Dr Dai is also a Senior Honorary Lecturer at the University of Auckland, principle supervisor of Paediatric Ophthalmology Fellowship and supervises PhD students.