Squint Club 2018
This year’s meeting of the Australian and New Zealand Strabismus Society (ANZSS), better known as the Squint Club, was held at the Sydney Eye Hospital, the oldest hospital in Australia dating back to 1788. Set in the historic sandstone Victorian building with ornate metal balustrades and stained-glass windows, it was a magnificent juxtaposition of the old and the new with the vibrant and modern city of Sydney being a few steps away.
This year’s event was well attended by 129 participants including ophthalmologists, fellows, registrars and orthoptists from mainly the Australasia region and one delegate from China. International guest speakers included: Dr Ramesh Kekunnaya, head of paediatric ophthalmology, strabismus and neuroophthalmology at LV Prasad Eye Institute in Hyderabad, India, and a member of the executive bureau of the World Society of Paediatric Ophthalmology and Strabismus; and Daisy Godts, chief orthoptist at the University of Antwerp in Belgium and council member of the International Orthoptic Association.
The 2018 meeting kicked off with a welcome address by Dr Craig Donaldson, president of ANZSS, followed by a series of complex strabismus case presentations with an expert panel discussion consisting of Dr Kekunnaya, Godts, Dr Donaldson (Sydney), Associate Professor James Elder (Melbourne) and Dr Wendy Marshman (Melbourne). This session was filled with “what to do”, “what not to do” and “what I should’ve done instead”, carried out in convivial manner where even senior ophthalmologists shared their learning pitfalls.
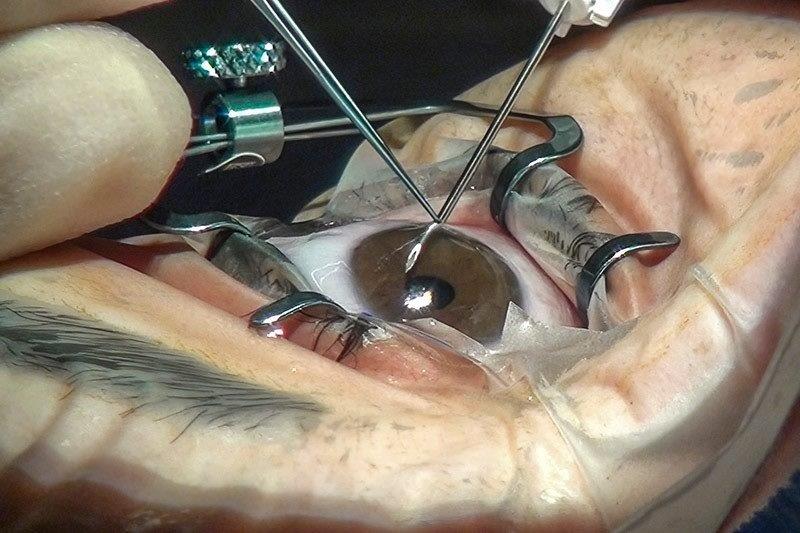
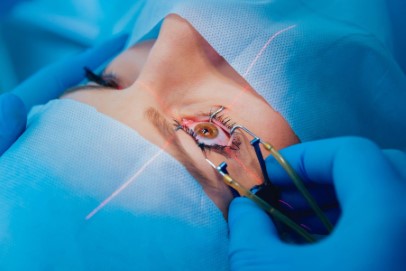
Dr Kekunnaya shared his experience in performing strabismus surgery under topical anaesthesia which is usually reserved for adult squint cases. It can be performed successfully with minimal discomfort, but patient selection is key, he said. Patients who can comfortably tolerate a cotton tip applicator soaked with topical anaesthesia on their conjunctival limbus are suitable candidates. Effective haemostasis can be aided by vascular vasoconstriction with topical brimonidine or phenylephrine at the beginning of surgery. Topical anaesthesia surgery can be useful in re-operation cases within 10 to 15 days of the first surgery, for example in cases of a slipped muscle, he added.
Motility examination of neurological patients is one of the least understood and inadequately performed ocular assessments for most ophthalmology trainees. This was succinctly covered in a practical and step-by-step manner by Daisy Godts in her refreshing back-to-the-basics lecture.
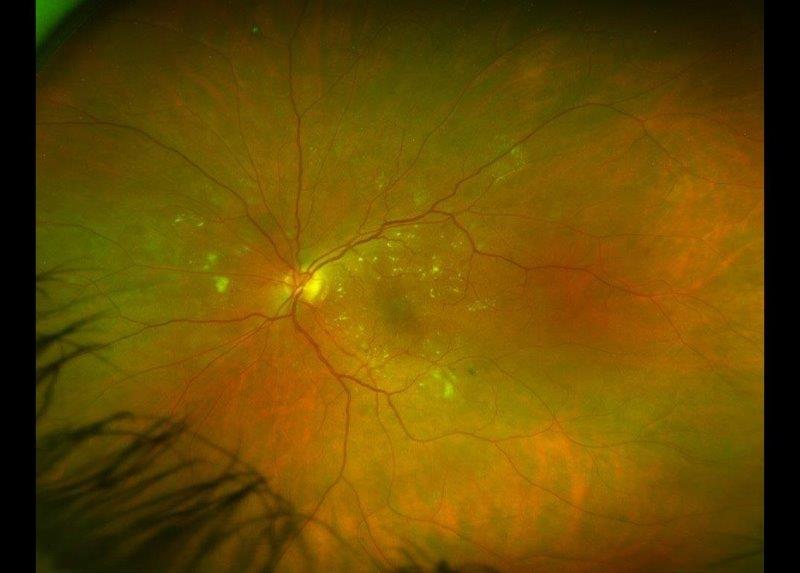
Dr Lionel Kowal from Melbourne presented, ‘MRI in Strabismus’, interestingly highlighting the role of radiological imaging of the extraocular muscles and its pulley system in squint assessment and surgical planning. It is particularly useful in cases of superior oblique palsy, abduction deficits and strabismus in high myopia to establish the underlying pathophysiological cause of each condition, which will help determine the appropriate surgical strategy, he said. Most importantly, is the interpretation of extraocular muscle system imaging and the need to further educate both ophthalmologists and radiologists on what is normal versus abnormal and whether the abnormal findings have any clinical significance.
Age-related distance esotropia which may be part of sagging eye syndrome is now a well-recognized diagnostic entity. Godts gave a comprehensive lecture on its diagnosis and long-term follow up where prismatic correction can be an effective initial therapy. However, the angle of deviation typically increases over time and larger doses of standard bilateral medical rectus recessions have been successful in Belgium.
The William Gillies Lecture was delivered by Dr Kekunnaya in a two-part series on Duane retraction syndrome (DRS), where he outlined the esotropic and exotropic types. He shared his review of an impressive 400+ patients with DRS and the principles of DRS strabismus surgery which is based on primary position of deviation, degree of anomalous head posture (AHP), severity of globe retraction and overshoots, degree of limitation of ductions and forced duction testing (FDT). Superior rectus transposition to the lateral rectus (LR), with or without medial rectus (MR) recession may be considered as an initial procedure in esotropic DRS as it has the advantage of improving abduction. However, there is a risk of inducing vertical or torsional deviation. Exotropic DRS is commonly associated with globe retraction and overshoots, hence LR and MR recessions in the affected eye with Y-splitting of LR are effective in addressing these issues.
The unique ‘live cases’ presentation was undeniably the crowd puller for this meeting where patients were examined by senior strabismologists including Professor Glen Gole (Brisbane) and Drs Lionel Kowal (Melbourne), Shuan Dai (Auckland), Ross Fitzsimons (Sydney), Kekunnaya and Daisy Godts, and video projected for the audience. Six highly-puzzling strabismus patients, including one who had travelled from Auckland, with either a diagnostic dilemma or challenging surgical management or both, were presented. A fruitful discussion between the experts and members of the audience helped formulate the best management strategies for these patients, be it active or inactive.
The social aspect of the meeting was not left unattended with the conference dinner being held at the iconic Sydney Tower, standing 1014 feet above the central business district and offering spectacular views of Sydney and its harbour. Participants enjoyed a delectable meal in a most amiable atmosphere with old and new acquaintances.
Overall, this year’s Squint Club meeting has maintained its reputation as a highly educational, engaging and congenial affair, and much credit goes to the organising committee, volunteer patients and ANZSS members. I hope the tradition continues and wish the Squint Club more prosperous meetings in the future under the new presidency of our own Auckland-based expert, Dr. Shuan Dai.
*Dr Malisa Ami is currently on one-year study leave from the National University of Malaysia as a fellow in paediatric ophthalmology at the University of Auckland.