The immune system, the nervous system and the ocular surface
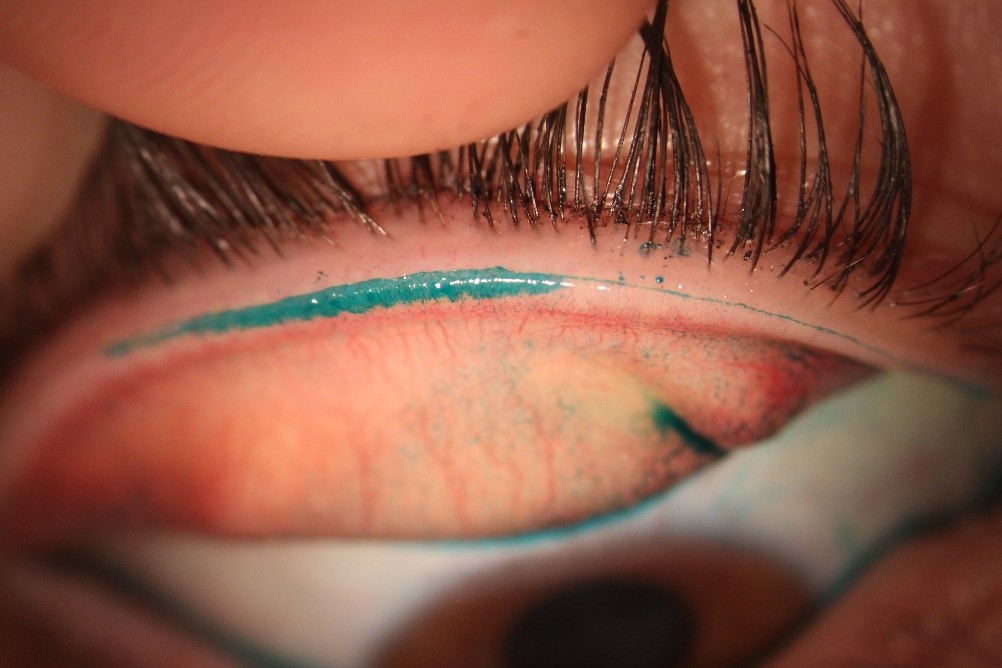
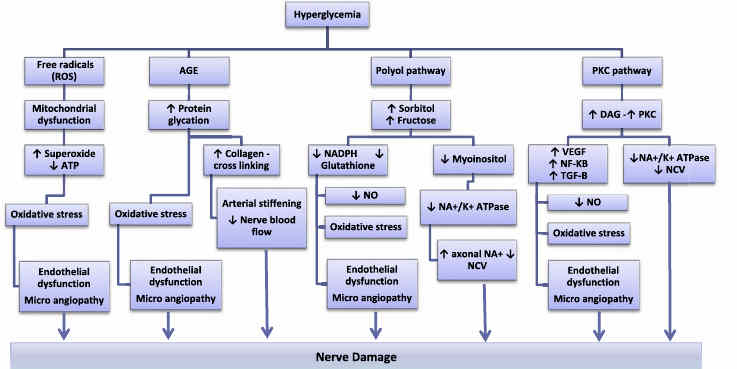
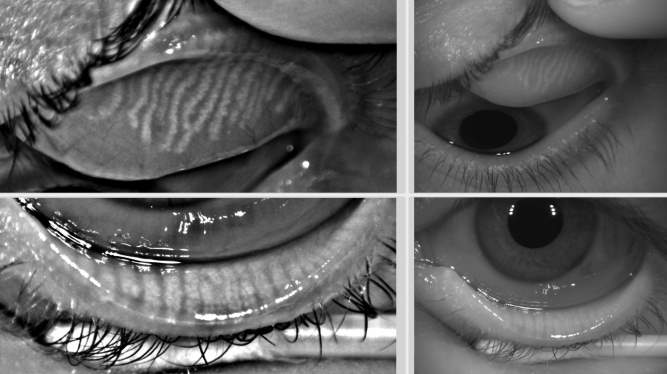
A characteristic of dry eye disease (DED) is the presence of inflammation, a significant driving factor of the vicious circle that is DED. TFOS second dry eye workshop (TFOS DEWS II) aptly described this process as being initiated by evaporative water loss leading to hyperosmolar tissue damage. This contributes to the inflammatory cascade, with an increased presence of inflammatory markers in the tear film, such as matrix metalloproteinase-9 (MMP-9). These changes cause damage to both epithelial and goblet cells, manifesting in the clinical signs of corneal and conjunctival staining and reduced tear break-up time. This further feeds into the initial hyperosmolarity, perpetuating the process. This cycle of events also causes damage to the corneal nerves which provide nutritional support to the corneal epithelium by releasing factors important for growth and wound healing, such as substance P. Epithelial cells reciprocate by providing support to corneal nerves by secreting growth factors that promote nerve growth. In DED, the equilibrium of these supporting growth factors and inflammatory markers is affected.
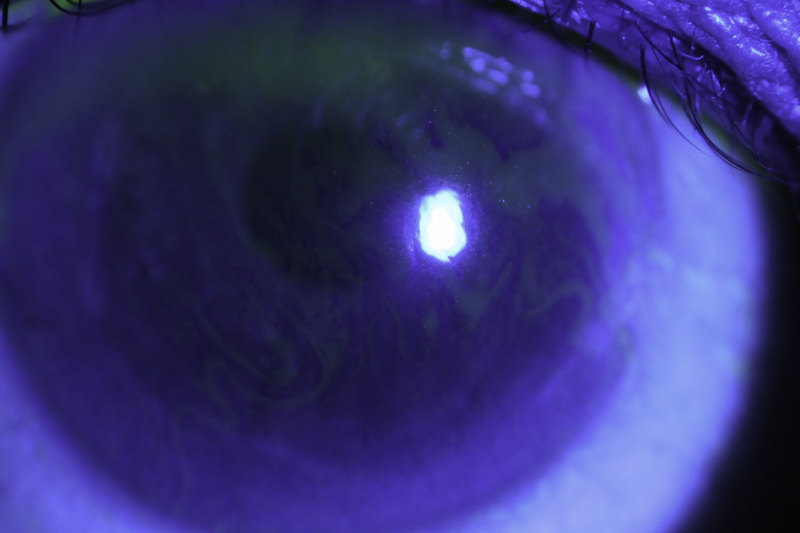
A possible relationship has been described between the ocular surface immune and nervous systems. To understand what impact DED has on these systems, it is important to first understand what is normal in the healthy eye. This can help us understand what we need to do to maintain the equilibrium of the ocular surface. To do this, we set out to understand the relationship between corneal nerve structure and the presence of inflammatory mediators and neuromediators in the tear film. We collected the tears of 21 healthy participants and also took images of their corneal nerves using an in vivo corneal confocal microscope. We found that neuromediator substance P in the tear film correlated with measures of nerve fibre morphology, where higher levels were associated with a greater number of nerves. We also found that higher levels of tissue-inhibitor of MMPs (TIMP-1) and the inflammatory mediator interleukin-6 (IL-6) were associated with a reduced presence of corneal nerves. These results confirm the immune and nervous systems in the ocular surface are interlinked and that what affects one, may affect the other.
Another exciting finding from our research was that a higher number of hours spent sleeping meant a higher number of corneal nerves being present, and more hours spent exercising was associated with thicker corneal nerves. This reinforces the need for a greater understanding into the impact that exercise and sleep have on the nervous system and the impact that such modifiable factors might have on ocular health.
With the understanding of the healthy ocular surface, we can now look towards understanding how this changes in DED and work towards restoring its equilibrium.
References
Chotikavanich, S, CS de Paiva, Q Li de, JJ Chen, F Bian, WJ Farley and SC Pflugfelder (2009). “Production and activity of matrix metalloproteinase-9 on the ocular surface increase in dysfunctional tear syndrome.” Invest Ophthalmol Vis Sci 50(7): 3203-3209.
Bron, AJ, CS de Paiva, SK Chauhan, S Bonini, EE Gabison, S Jain, E Knop, M Markoulli, Y Ogawa, V Perez, Y Uchino, N Yokoi, D Zoukhri and DA Sullivan (2017). “TFOS DEWS II pathophysiology report.” Ocul Surf 15(3): 438-510.
Belmonte, C, JJ Nichols, SM Cox, JA Brock, CG Begley, DA Bereiter, DA Dartt, A Galor, P Hamrah, JJ Ivanusic, DS Jacobs, NA McNamara, MI Rosenblatt, F Stapleton and JS Wolffsohn (2017). “TFOS DEWS II pain and sensation report.” Ocul Surf 15(3): 404-437.
Muller, LJ, CF Marfurt, F Kruse and TM Tervo (2003). “Corneal nerves: structure, contents and function.” Exp Eye Res 76(5): 521-542.
Cruzat, A, D Witkin, N Baniasadi, L Zheng, JB Ciolino, UV Jurkunas, J Chodosh, D Pavan-Langston, R Dana and P Hamrah (2011). “Inflammation and the nervous system: the connection in the cornea in patients with infectious keratitis.” Invest Ophthalmol Vis Sci 52(8): 5136-5143.
Dr Maria Markoulli is an optometrist and senior lecturer at the University of New South Wales School of Optometry and Vision Science. Dr Luisa Colorado is a post-doctoral research fellow and Dr Katie Edwards a lecturer at the School of Optometry and Vision Science at the Queensland University of Technology.