Wound-healing eye drops
Scientists at the University of Birmingham have developed an eye drop consisting of a fluid gel, loaded with a natural wound-healing protein called decorin, that can help prevent or minimise vision loss through scarring of the cornea.
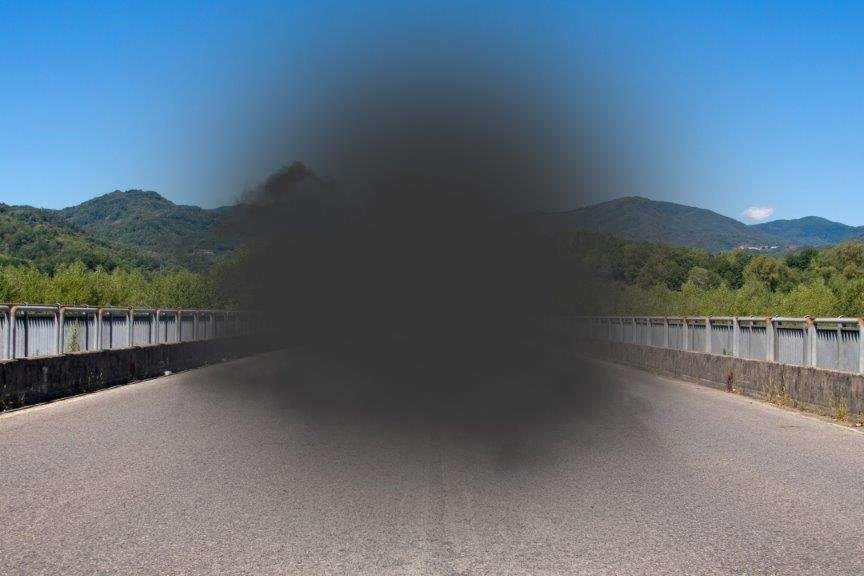
The surface of the eye is usually transparent but scars resulting from eye infection or trauma make it opaque, causing blurred vision, or in extreme cases, complete blindness.
Pre-clinical research, published in Regenerative Medicine, shows that the eye drop speeds healing, reduces scarring and improves corneal transparency within a matter of days when treating Pseudomonas aeruginosa, an eye infection commonly associated with poor contact lens hygiene.
The current standard of care for eye infection is eye drops containing antibiotics and corticosteroids to reduce inflammation, followed by intensive lubrication to prevent further damage to the eye during blinking. These treatments effectively sterilise the eye, although some patients are left with visual ‘hazing’ due to scars on the cornea. The only option to correct this is a surgical intervention, such as a corneal transplant.
Joint lead researcher, inflammation specialist Professor Ann Logan, said “this innovative fluid gel in the eye drop is designed to retain the decorin on the surface of the eye, and form a ‘therapeutic bandage’ that promotes scarless healing”.
Co-lead researcher, chemical engineer Professor Liam Grover added, “The fluid gel is a novel material that can transition between a solid and liquid state. This means it contours itself to the surface of the eye, is retained there, and is only slowly removed by blinking.” This research has shown for the first time that the fluid gel has a therapeutic effect in its own right, and the researchers believe it forms a barrier that protects the surface of the eye from further damage caused by blinking.
Dr Lisa Hill, from the university’s Institute of Clinical Sciences, says, “The anti-scarring eye drop has the potential to vastly improve outcomes for patients with eye infection and trauma. It could also help save many people’s sight, particularly in the developing world where surgical interventions such as corneal transplants are not available.”