When should you check for dry eye?
Should we look for dry eye on every patient? I get this question with some frequency. I admit I find it perplexing. I am reminded of a practitioner asking me several years ago if I did biomicroscopy on every patient. Well, of course! Do I look for dry eye disease on every patient? The answer is a resounding YES! Allow me to explain why.
There's a lot of it
It is well-established that dry eye disease (DED) is prevalent¹. We often hear that it is ‘multifactorial’. What does that mean precisely? It means that many roads lead to DED and that's why there are so many dry eye sufferers. Some common culprits are age, sex, medications, device use, topical preservatives, nutrition, environment, migraine, ophthalmic surgery, autoimmune disease and meibomian gland dysfunction. Does this sound like your patient base?
While postmenopausal women are highest on the suspect list for dry eye, device use and medications are two of the more common causes of symptoms in younger people. A 2016 study looked at 630 subjects, of which 60 had both signs and symptoms of DED. Thirty of these stopped all smartphone use for four weeks and their rate of dry eye went from 100% to 0%. While that statistic is undoubtedly impressive, even more shocking is the age range of the subjects: seven to 12 years old²!
When reviewing patient medications meanwhile, antidepressants and antipsychotics have the highest odds of causing dry eye disease³. A 2014 Australian paper found a significant increase in the prescribing of antidepressants, antipsychotic and ADHD medications between 2009 and 2012. For children aged 10-14, antidepressant and antipsychotic dispensing went up 36% and 49% respectively. For patients aged 20-24 years old, ADHD medication was prescribed 71% more⁴.
It affects vision
My personal introduction to the visual effects of DED was during my own LASIK consultation, where it was revealed that I had higher-order aberrations. As a low spherical myope, that didn't make sense. The surgeon treated me for dry eye and within two weeks the aberrations were gone. This was an epiphany - the tear film affects vision⁵! This is something I had overlooked. I started thinking of dry eye as a ‘vision disease’ and, as a ‘vision doctor’, I decided to look for dry eye on every patient.
It affects quality of life
Once simply viewed as a nuisance, dry eye is now recognised as a disease. Patients with dry eye may have difficulty reading, driving, watching television and other activities of daily living⁶. Using a 30-minute, 7200-word passage, Akpek et al found that dry eye patients with corneal damage read nearly 28 words per minute slower compared with ‘normals’, while their reading speed correlated with the amount of corneal staining⁷. As we all aim to reduce dry eye symptoms, keep in mind that a clear cornea is also a worthwhile goal.
There are many treatment options
Before 2003, artificial tears and warm compresses were about the only options we could offer dry eye-suffering patients. Fast forward to 2020 and, in the US at least, we have three prescribed dry eye medications, three in-office meibomian gland expression devices, amniotic membranes, autologous serum eye drops and numerous other choices; recently, a topical medication for neurotrophic keratitis was released. And the therapeutic pipeline is strong: look soon for a topical prescription eye drop for blepharitis, a keratolytic for meibomian gland dysfunction and more preservative-free eye drop delivery systems.
Treating DED helps both patient and practice
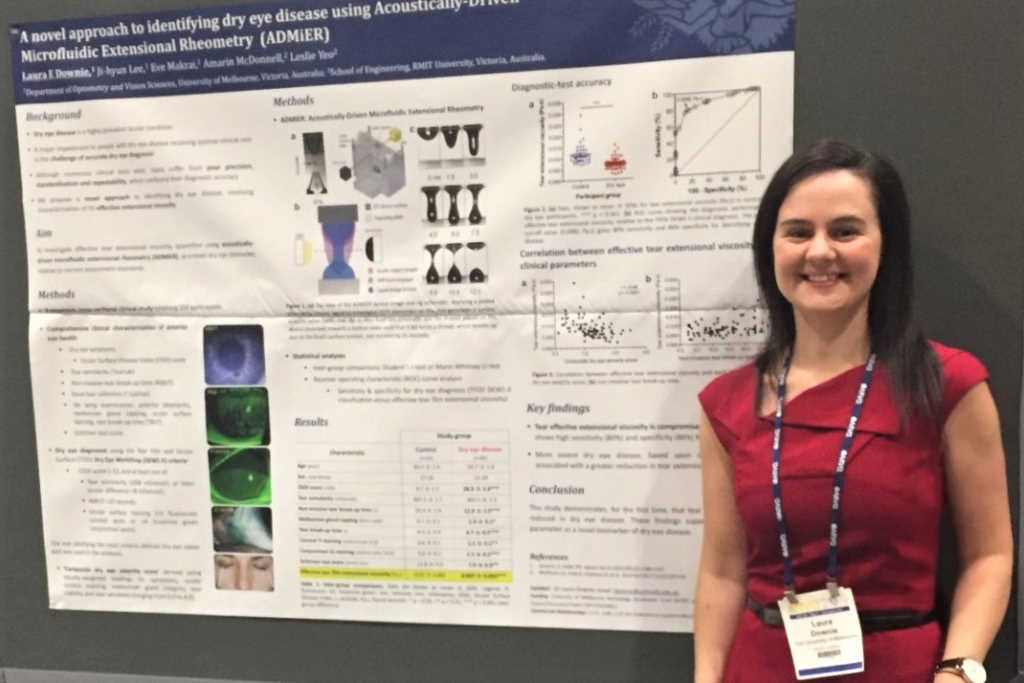
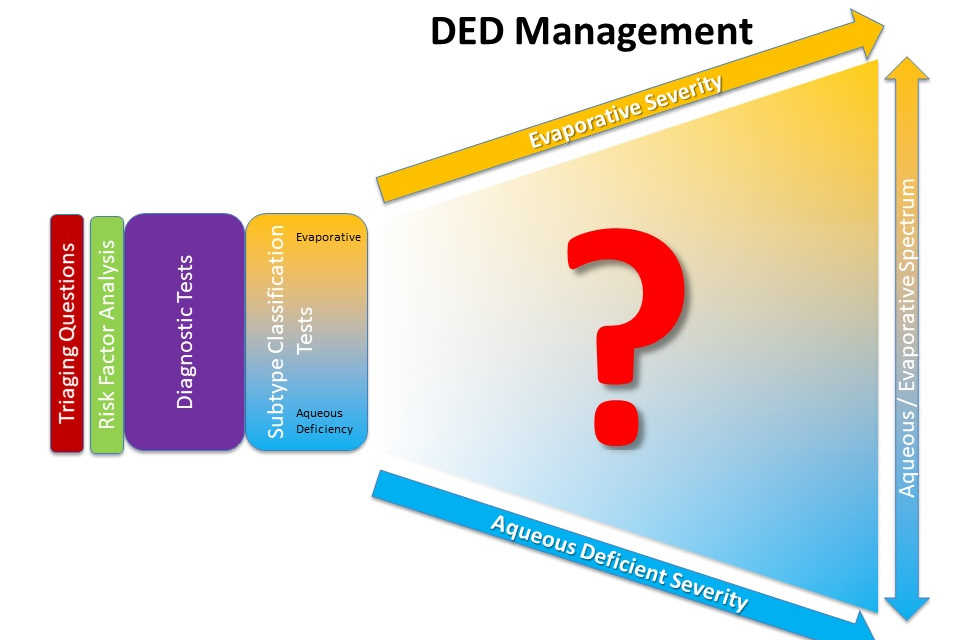
As a result of my ‘vision disease’ epiphany, I implemented an algorithm to screen, diagnose and treat dry eye. Within six months, therapeutic practice visits tripled, while revenue per patient remained the same.
I am often introduced as a practitioner who is ‘aggressively’ diagnosing and treating ocular surface disease. Rather, I am actually ‘appropriately’ doing so. I simply follow expert recommendations, which I had been oblivious to previously. My algorithm was initially based on the TFOS Dry Eye Workshop of 2007 and has since evolved with the 2017 TFOS DEWS II update. I strongly recommend TFOS DEWS II as a starting point for diagnosing and treating dry eye; it is an evidence-based consensus with a stepwise treatment protocol.
While my approach is backed by science, it is also ‘streamlined’ to be efficient and straightforward, to ensure it is sustainable in practice.
Weekly, patients thank us for taking the extra time to address their complaints which remained unaddressed by other practitioners. As a result, we get many patient referrals and practitioner consults as well. Becoming a local ‘dry eye clinic’ can be a significant practice builder.
In conclusion
So, should you look for dry eye on every patient? Yes, yes, yes! As vision care providers, vision begins at the tear film. With such a high prevalence, as well as impact on vision and quality of life, you owe it to your patients to take a look and, if treating dry eye patients is not for you then send them to someone who does. Your patients deserve it!
References
- Nelson JD, Craig JP, Akpek EK, et al. TFOS DEWS II Introduction. Ocul Surf. 2017;15(3):269-275.
- Moon, J.H., Kim, K.W. & Moon, N.J. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: a case control study. BMC Ophthalmol 16 (1), 188.
- Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II Iatrogenic Report. Ocul Surf. 2017;15(3):511-538.
- Karanges EA, Stephenson CP, McGregor IS. Longitudinal trends in the dispensing of psychotropic medications in Australia from 2009-2012: focus on children, adolescents and prescriber specialty. Aust N Z J Psychiatry. 2014;48(10):917-931.
- Montes-Mico R, Caliz A, Alio JL. Wavefront analysis of higher-order aberrations in dry eye patients. J Refract Surg 2004;20:243-7
- Uchino M, Schaumberg DA. "Dry Eye Disease: impact on quality of life and vision." Curr Ophthalmol Rep. 2013; 1(2): 51-57.
- Karakus S, Mathews PM, Agrawal D, et al. Impact of dry eye on prolonged reading. Optom Vis Sci. 2018 Dec;95(12):1105-1113.
Dr Scott Schachter founded Advanced Eyecare and Eyewear Gallery Optometry in 1994 in Pismo Beach, California. He has published and presented many papers on the ocular surface, is a regular columnist for Optometry Times and Ocular Surface News and is one of eight US global ambassadors for the Tear Film and Ocular Surface Society (TFOS).