AMD stem cell trials and big data
Phase I clinical study of an embryonic stem cell–derived retinal pigment epithelium patch in AMD, Da Cruz, et al.
Nature Biotechnology, 19 March 2018
Review: This is the most significant breakthrough in the use of stem cells for the treatment of macular diseases and this paper generated much publicity around the world. It is not uncommon now for patients to ask me if stem cell therapy will be suitable for their macular conditions.
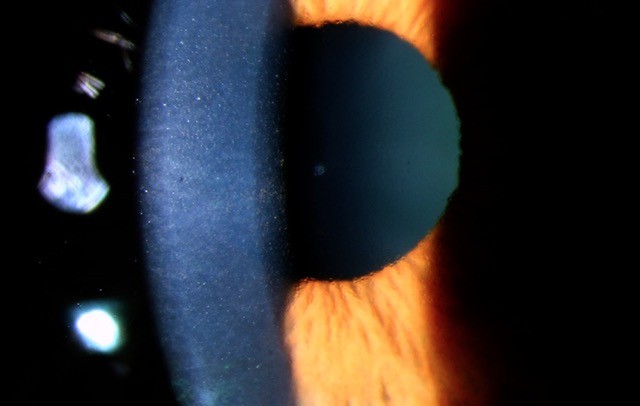
The original paper is complex and details the development of the human embryonic stem cell (hESC)-derived RPE monolayer patch, animal studies and a phase I study on two patients with wet age-related macular degeneration (AMD). Previous studies on hESE-RPE involved direct injection of a hESE-RPE cell suspension into the sub-retinal space, which resulted in no significant improvement in retinal structure and function. The technological breakthrough in this paper is the development of a therapeutic, biocompatible hESC-RPE monolayer on a coated-synthetic membrane - herein, termed ‘the patch’ - for transplantation. The hESE-RPE cells on the patch are delivered fully differentiated, polarised and with a tight junction barrier formed.
Teratoma risk was addressed in a mouse model, showing that injection of undifferentiated-hESE cell suspension can result in the formation of teratoma, but this was not observed with the injection of differentiated-hESE-RPE cell suspension. The safety of the implantation of the hESE-RPE patch was established in a pig model (as mouse eyes are too small for this purpose) prior to the phase I study.
10 patients with wet AMD were recruited for this study and the paper reported overwhelmingly positive results in the first two patients. Both patients had severe wet AMD not amenable to anti-VEGF (severe sub-macular and sub-RPE haemorrhage) with poor visual prognosis pre-operatively. One hESE-RPE patch was placed in the sub-retinal space, under the fovea, in the affected eye of each patient. In both patients, hESC–RPE was present over the full area of the patch at 12 months.
The early treatment diabetic retinopathy study letter chart was used to define the mean best-corrected visual acuity (BCVA) which improved over 12 months from 10 to 39 and from eight to 29 letters, in patients one and two, respectively. Microperimetry showed visual fixation at the centre of the patch and vision over the patch in both patients. Reading speed improved from 1.7 to 82.8 and from 0 to 47.8 words/min in patients one and two, respectively, over 12 months using the University of Minnesota MNRead test, an improvement and final level not found in the sub-macular surgery trial.
Three serious events were reported, but none of these were related to the hESE-RPE patch and only local immunosuppression is required for the long-term survival of the hESE-RPE patch (fluocinolone acetonide intravitreal implant).
Comment: Despite the very encouraging result, I would like to see the outcome of the other eight patients enrolled in this study to know how effective this treatment is. To my patients, with currently untreatable macular disorders, I would tell them stem cell therapy is promising and I am cautiously optimistic that a stem cell-based treatment will be available in the foreseeable future.
Transplantation of human embryonic stem cell-derived retinal pigment epithelial cells in macular degeneration, Mehat, et al.
Ophthalmology, 5 June 2018
Review: This is a more recent study on the use of hESE-RPE cells in the treatment of molecular confirmed ABCA4 Stargardt disease (STGD). In contrast to the previous study, an hESE-RPE patch was not used here. The hESE-RPE cells were directly injected into the sub-retinal space as a suspension in an area just outside the vascular arcade, in a region extending from relatively well-preserved functional retina across a transitional zone of progressive degeneration to an area of atrophic non-functional retina, in 12 patients.
The hESE-RPE cell injection was shown to be safe (primary endpoint). Although there was increased pigmentation at the site of the injection, however, there was no conclusive evidence that the injected hESE-RPE cells were viable. Extensive testing with microperimetry and electro-diagnostics did not show any improvement in visual function.
Comment: It appears that without a bioengineered scaffold, direct sub-retinal injection of hESE-RPE cells is unlikely to be a viable avenue for the treatment of macular diseases.
The 2016 American Academy of Ophthalmology IRIS registry database, Chiang, et al.
Ophthalmology, 15 January 2018
Review: One of the latest trends in medical and ophthalmic research is the application of ‘big data’. This is fuelled by the development of electronic medical record systems (EMR), allowing data to be pulled automatically; efficient data storage systems; and vastly improved computational power and algorithms (machine learning).
The 2016 IRIS (Intelligent Research in Sight) registry database consists of 17,363,018 unique patients from 7,200 United States-based ophthalmologists. This large-scale dataset can be used to answer questions about practice patterns, disease prevalence, clinical outcomes and the comparative effectiveness of different treatments.
Several studies have been published using the IRIS data¹,² and rare events, such as post-operative endophthalmitis, can be studied in more detail with a big data approach than in a traditional clinical study. However, using this big data approach without context can lead to erroneous conclusions. For example, a data-driven analysis done by a major hospital misclassified patients with both pneumonia and asthma at a lower risk of death than those with pneumonia without asthma³, contrary to accepted clinical wisdom. The reason for the misclassification was that patients with asthma that developed pneumonia in that particular institute were directly admitted to the intensive care department, which led to better outcomes, but this was not captured by the data alone.
Comment: The IRIS registry is an exciting development and I expect many more papers from this dataset. However, the results of these big data studies must be interpreted in light of clinical experience and with caution.
References
Repka, M. X., Lum, F. & Burugapalli, B. Strabismus, Strabismus Surgery, and Reoperation Rate in the United States. Ophthalmology (2018).
doi:10.1016/j.ophtha.2018.04.024
Parke, D. W. & Lum, F. Return to the Operating Room after Macular Surgery. Ophthalmology (2018). doi:10.1016/j.ophtha.2018.01.009
Cabitza, F., Rasoini, R. & Gensini, G. F. Unintended Consequences of Machine Learning in Medicine. JAMA 318, 517 (2017).
About the author
Dr Leo Sheck practices at the Greenlane Clinical Centre in Auckland. After completing his ophthalmology training in New Zealand, he spent two years at Moorfields Eye Hospital with fellowship training in medical retina, genetics, uveitis and electro-diagnostics. Concurrently, he completed an MBA from Cambridge University on the use of artificial intelligence in healthcare.