Antiparasitic efficacy of eyelid cleansers for Demodex blepharitis
Ocular surface infestation with Demodex mites is recognised as a significant risk factor for the development of chronic blepharitis. Although 50% tea tree oil (Melaleuca alternifolia) is currently the mainstay for anti-demodectic treatment, it can cause considerable ocular irritation, restricting its use to brief in-office application.
This article briefly reviews the relationship between ocular Demodex and blepharitis, as well as two recent studies conducted by the University of Auckland Ocular Surface laboratory exploring the anti-demodectic efficacy of commercially-available eyelid cleansers and manuka honey.
Blepharitis is among the most commonly encountered ophthalmic conditions in clinical practice, affecting up to 47% of patients presenting to eye care practitioners. The condition is characterised by chronic inflammation of the eyelids and is recognised to have profound impacts on ocular comfort, vision and quality of life. It is commonly associated with signs and symptoms of ocular surface irritation, dry eye syndrome, intermittent visual disturbance, conjunctival hyperaemia, palpebral erythema and eyelid crusting. In severe cases, the inflammatory processes can also contribute to the development of irreversible sight-threatening corneal damage.
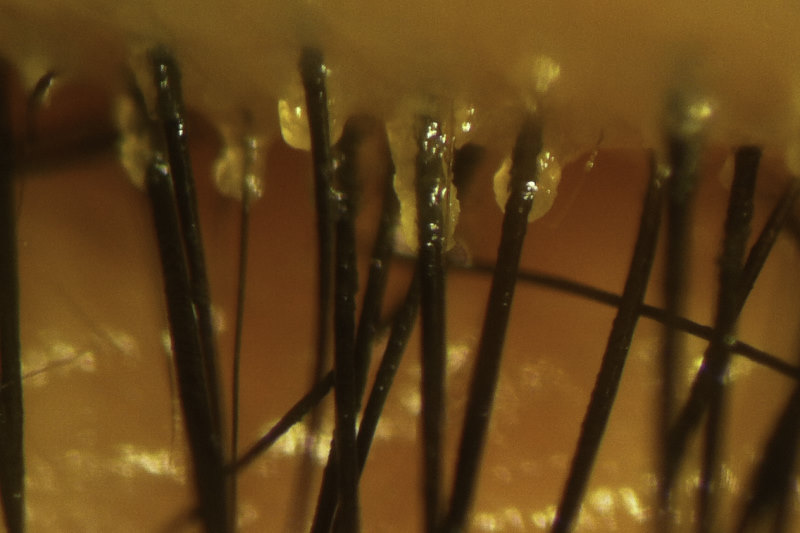
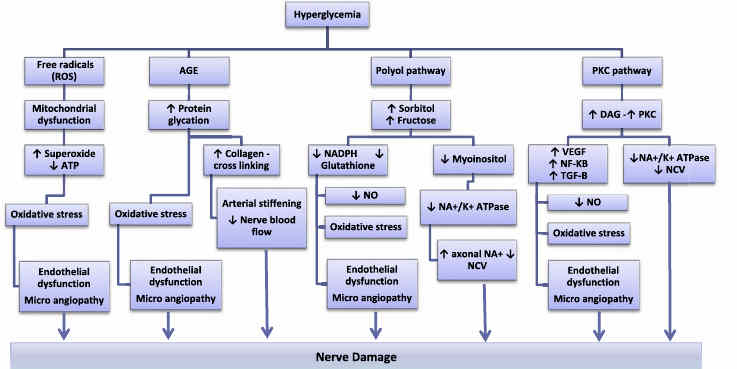
Although the complex pathophysiological mechanisms underlying the development of chronic blepharitis are not fully understood, recent research would suggest that ocular infestation with Demodex might be an important cause. Indeed, ocular demodicosis is observed in up to 68% of patients with chronic blepharitis and 60% of those with meibomian gland dysfunction, the most common subtype of posterior blepharitis. Infestation with Demodex folliculorum and Demodex brevis species (Fig 1), predominantly in the eyelash follicles and meibomian glands respectively, is thought to trigger an over-activation of host immune and inflammatory responses through a number of different mechanisms. Mechanical obstruction of the eyelash follicles and meibomian glands, as well as direct consumption and physical damage of the epithelium by the sharp appendages of the Demodex mites can directly induce inflammatory cascades. The associated reduction in the quality and quantity of meibomian gland secretions may also exacerbate aqueous tear evaporation, leading to tear film instability, hyperosmolarity, and ocular surface inflammation. In addition, chitin (the main constituent of the Demodex exoskeleton), as well as mite break-down products are strongly antigenic in some individuals. Finally, Demodex mites are also a potential vector for bacteria, especially Bacillus oleronius, and ocular infestation can contribute to bacterial hypercolonisation of the eyelids.
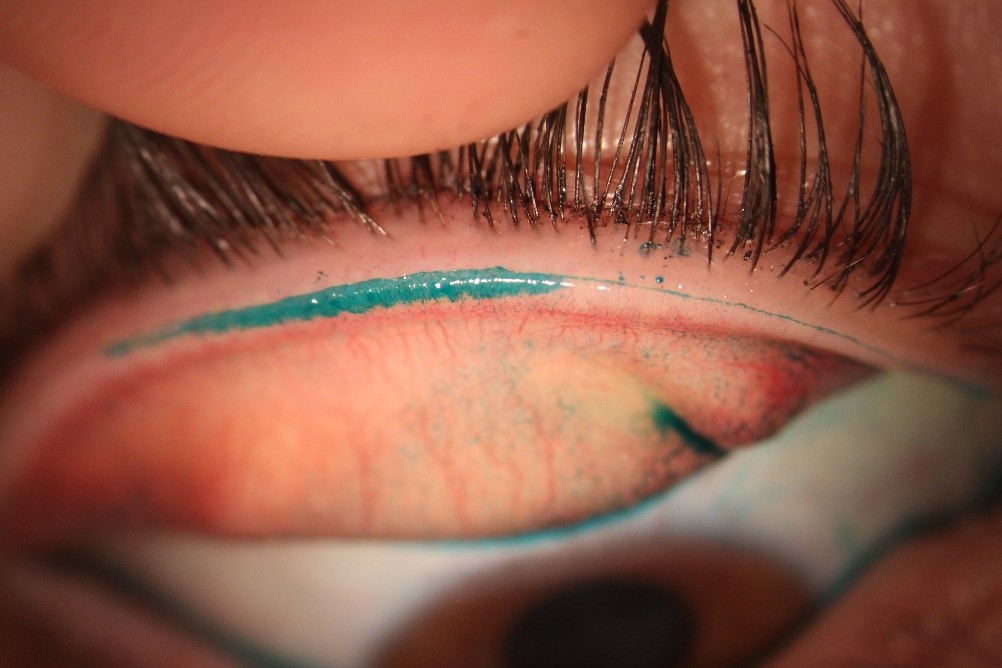
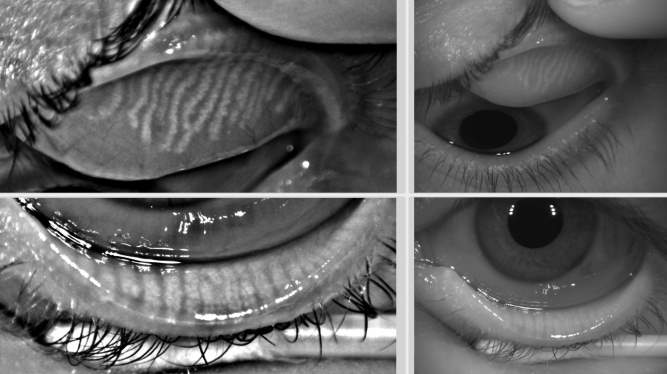
The diagnosis of ocular demodicosis is usually made clinically by the pathognomonic observation of cylindrical eyelash collarettes under slit lamp bio-microscopy (Fig 2), although the examination of epilated eyelashes for the presence of mites under light microscopy remains the gold standard diagnostic test. Treatment with 50% tea tree oil is the current mainstay for demodectic blepharitis management, although the considerable ocular irritation triggered by topical application limits its use to brief in-office application periods of less than 30 minutes. Self-administered eyelid cleansing formulations containing lower concentrations are usually recommended for patient use during intervening periods. The anti-demodectic efficacy of tea tree oil is thought to be primarily mediated by its terpinen-4-ol constituent, although the exact mechanisms by which inhibition of Demodex viability occurs has not yet been fully established.

Fig 2. Adult Demodex brevis
Anti-demodectic efficacy of commercial eyelid cleansers
A number of dedicated eyelid cleansing formulations are available commercially and are marketed to facilitate ocular hygiene in the management of chronic blepharitis. However, the antiparasitic efficacy of these topical formulations has not been previously established. A recent in vitro study conducted by the University of Auckland Ocular Surface Laboratory compared the anti-demodectic activity of four commercially available dedicated eyelid cleansers (Cliradex towelette cleanser, Oust Demodex cleanser, Blephadex eyelid foam and TheraTears SteriLid eyelid cleanser) with 50% tea tree oil. The study also sought to identify and quantify the active antiparasitic constituents of the commercial formulations.
Consistent with the results of earlier studies, potent antiparasitic activity of undiluted terpinen-4-ol was observed against ocular Demodex mites acquired from epilated eyelashes of blepharitis patients. Interestingly, linalool, a constituent of TheraTears SteriLid, was found to exhibit comparable anti-demodectic efficacy to terpinen-4-ol in its undiluted form. The specific antiparasitic activity of linalool against ocular Demodex has not been previously described in the literature and this novel finding would support future clinical studies exploring the efficacy of linalool-based formulations in the management of demodectic blepharitis.
Although anti-demodectic activity was demonstrated by all four commercial eyelid cleansers, the Cliradex towelette cleanser was the only formulation that demonstrated comparable antiparasitic efficacy to 50% tea tree oil. This was thought to be potentially related to Cliradex containing the highest terpinen-4-ol content among the commercial formulations.
Anti-demodectic efficacy of manuka honey
Natural honey is well known for its anti-inflammatory and antimicrobial capacities, which is likely attributed to its low pH, high osmolarity hydrogen peroxide content, and non-peroxide constituents, including methylglyoxal. New Zealand native manuka (Leptospermum scoparium) honey, in particular, has gained significant interest in recent years, due to its high concentrations of methylglyoxal, which is recognised to be more resistant to inactivation by heat and catalases then antimicrobial peroxide constituents. A cyclodextrin-complexed microemulsion formulation of MGO manuka honey has recently been developed for overnight topical eyelid application and is currently under investigation with regard to its to ocular hygiene potential in the clinical management of blepharitis. The eyelid cream has been observed to exhibit manuka honey in vitro anti-bacterial activity against ocular microbiota and successfully underwent safety and tolerability testing in a two-week randomised masked clinical trial of healthy human participants.
The in vitro anti-demodectic activity of MGO manuka honey was compared with 50% tea tree oil in a recently published study conducted by the University of Auckland Ocular Surface Laboratory. The findings demonstrated that cyclodextrin-complexed manuka honey exhibited comparable antiparasitic efficacy to 50% tea tree oil against ocular Demodex mites acquired from blepharitis patients. Together with the results from the earlier clinical tolerability trial, this would suggest that manuka honey shows the potential to offer an alternative non-irritating topical treatment to 50% tea tree oil. Clinical trials exploring the efficacy of manuka honey in demodectic and non-demodectic blepharitis are already underway.
Conclusions
Ocular surface infestation with Demodex mites is emerging as a significant cause of chronic blepharitis. Topical 50% tea tree oil formulations are the current mainstay of treatment for demodectic blepharitis, although the significant ocular irritation restricts its use to brief application periods under clinical supervision. A recent study conducted by the University of Auckland Ocular Surface Laboratory demonstrated antiparasitic activity of four commercially available, dedicated eyelid cleansers, although among the formulations tested, only Cliradex exhibited comparable efficacy to 50% tea tree oil. A separate study showed that comparable anti-demodectic activity was observed between MGO manuka honey and 50% tea tree oil, which would suggest promise for complexed manuka honey to offer an alternative non-irritating topical treatment for ocular Demodex infestation.
References
- Nicholls SG, Oakley CL, Tan A, Vote BJ. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017;37(1):303-312.
- Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular Surface Discomfort and Demodex: Effect of Tea Tree Oil Eyelid Scrub in Demodex Blepharitis. J Korean Med Sci. 2012;27(12):1574-1579.
- Cheung IMY, Xue AL, Kim A, Ammundsen K, Wang MTM, Craig JP. In vitro anti-demodectic effects and terpinen-4-ol content of commercial eyelid cleansers. Contact Lens Anterior Eye. 2018 (in press).
- Frame K, Cheung IMY, Wang MTM, Turnbull PR, Watters GA, Craig JP. Comparing the in vitro effects of MGO™ Manuka honey and tea tree oil on ocular Demodex viability. Contact Lens Anterior Eye. 2018 (in press).
- Duncan K, Jeng BH. Medical management of blepharitis. Curr Opin Ophthalmol. Jul 2015;26(4):289-294.
- Sung J, Wang MTM, Lee SH, Cheung IMY, Ismail S, Sherwin T, Craig JP. Randomized double-masked trial of eyelid cleansing treatments for blepharitis. Ocul Surf. 2018;16(1):77-83.
- Liu J, Sheha H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Cl. 2010;10(5):505-510.
- English FP, Nutting WB. Feeding characteristics in demodectic mites of the eyelid Aust J Opthalmol. 1981;9(4):311-313.
- Kim JH, Chun YS, Kim JC. Clinical and Immunological Responses in Ocular Demodecosis. J Korean Med Sci. 2011;26(9):1231-1237.
- Gao YY, Di Pascuale MA, Li W, et al. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmol. 2005;89(11):1468-1473.
- Gao Y-Y, Di Pascuale MA, Elizondo A, Tseng SCG. Clinical Treatment of Ocular Demodecosis by Lid Scrub With Tea Tree Oil. Cornea. 2007;26(2):136-143.
- Kheirkhah A, Casas V, Li W, Raju VK, Tseng SC. Corneal manifestations of ocular demodex infestation. Am J Opthalmol. 2007;143(5):743-749.
- Craig JP, Rupenthal ID, Seyfoddin A, Cheung IMY, Uy B, Wang MTM, Watters GA, Swift S. Preclinical development of MGO Manuka Honey microemulsion for blepharitis management. BMJ Open Ophthalmol. 2017;1(1):e000065.
- Craig JP, Wang MTM, Ganesalingam K, Rupenthal ID, Swift S, Loh CS, Te Weehi L, Cheung IMY, Watters GA. Randomised masked trial of the clinical safety and tolerability of MGO Manuka Honey eye cream for the management of blepharitis. BMJ Open Ophthalmol. 2017;1(1):e000066.
Dr Michael Wang is a part-time PhD student in the Department of Ophthalmology at the University of Auckland, under the supervision of A/Prof Jennifer Craig.