Artificial tears: preserved or non-preserved, that is the question
With apologies to William Shakespeare for the title, this was indeed the question addressed in our recent literature review1. With increasing availability and focus on preservative-free drops, eye care practitioners have been left wondering if preserved artificial tears continue to have a place in the treatment of dry eye disease (DED).
Any multidose drop must have some way of maintaining its sterility throughout its intended length of use. Preservatives are antimicrobial agents and are used in multidose drops for this purpose. They must balance an ability to be efficacious against a wide variety of pathogens, whilst minimising their toxic effects on the cells of the ocular surface2. Treatment and symptom alleviation of DED may require dosing of drops several times a day, over a period of many years. Any agents included in dry eye therapies must minimise their impact on an ocular surface that is already compromised.
Preservatives to avoid
In all fairness, the concern about the impact of preservatives on the ocular surface, especially the potentially compromised ocular surface of the dry eye patient, is founded on good evidence. Specifically, the impact of benzalkonium chloride (BAK) is widely understood, with its detrimental effects accumulating over time in a dose-dependent manner1. Those adverse changes are experienced by the user as discomfort on instillation, burning, stinging and foreign body sensation, dry eyes, tearing and itchy eyelids3. BAK acts directly on cells including those of the ocular surface, inducing clinical signs such as superficial punctate keratitis, conjunctival hyperemia, blepharitis3,4, increased osmolarity5,6, reduced tear production7,8 and reduced tear film break-up time7,8. At the cellular level, BAK reduces the number of goblet cells and increases inflammatory responses9,10. When the actions of BAK are viewed in light of the definition of DED (which recognises the loss of tear film homeostasis as a central characteristic)11, it is easy to conclude that use of BAK-preserved drops should be avoided in dry eye disease, regardless of the severity1,12.
Alternative preservatives
Our review examined the ocular surface compatibility evidence base for a range of non-BAK alternative preservatives. These alternatives fall broadly into two categories: quaternary compounds and oxidising preservatives.
Polyquaternium-1 (Polyquad, Alcon) is a hydrophilic, cationic quaternary compound that is around 27 times larger than BAK and has a different mode of action13. In studies, although some cell changes have been seen in vitro14, it consistently results in significantly less disruption to the ocular surface than BAK-preserved formulations2,15-17. Oxidising preservatives maintain antimicrobial properties in solution, decomposing to harmless by-products once applied to the eye. Examples include stabilised oxychloro complex (Purite, Allergan; OcuPure, Johnson & Johnson), and sodium perborate (GenAqua, Alcon). Previous review papers highlight the lack of studies on some preservatives in this group, but in general conclude that they have significantly less effect on the ocular surface than BAK2,18.
Preservative-free formulations
Preservative-free formulations often come in single-use vials. Multidose preservative-free drops are also available, where use is made of specialised bottles designed to prevent contamination. Preservative-free drops result in low levels of ocular surface disruption, with significant improvements in signs and symptoms and fewer cellular changes compared to BAK-preserved drops3,19-23. Depending on study design, preservative-free drops either show no significant difference in performance compared to non-BAK preservatives24-26, or cause less disruption than preserved formulations17,19,27.
In practice
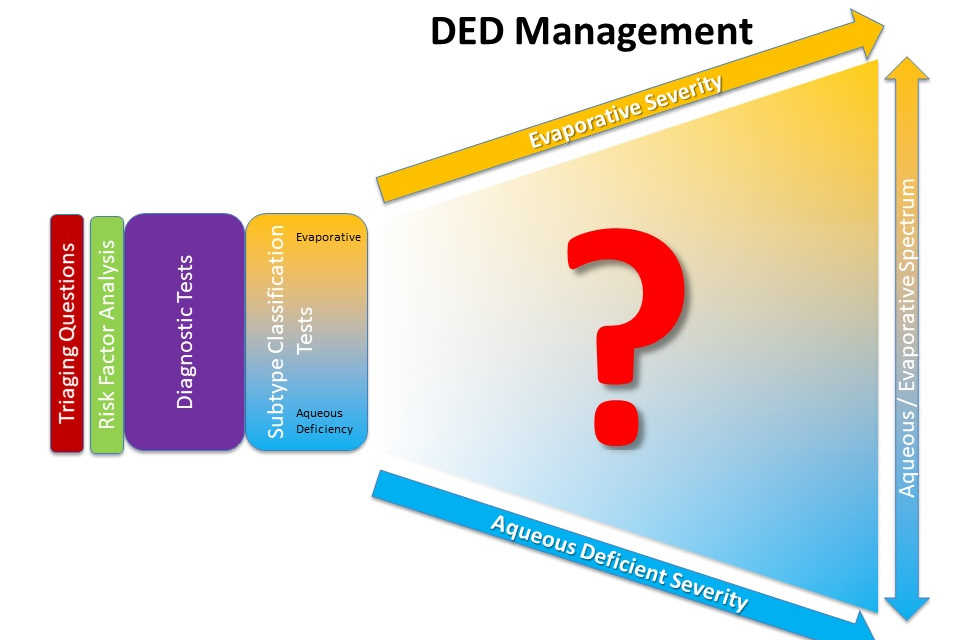
Evidence suggests that the use of BAK-preserved drops should be avoided in all patients with dry eye disease. The first step in the TFOS DEWS II staged management approach suggests the most appropriate ocular lubricant from the range of non-BAK preserved options be recommended12. If those measures are inadequate, step two recommends the use of preservative-free drops for patients with significant ocular surface disruption or severe DED12. Finally, given that 86% of patients with DED have signs of meibomian gland dysfunction28, the main contributor to evaporative dry eye, lipid-containing or lipid-stabilising drops can be particularly helpful. There is currently a relatively limited choice of preservative-free, lipid-containing options.
That makes the conclusion to our review, and the answer to the opening question, important. Yes, both types of drops can be considered for most dry eye patients; there is a place in the treatment of dry eye disease for both non-BAK preserved and preservative-free formulations. This evidence-based conclusion enables the eye care practitioner to work with individual patients to recommend the most appropriate formulation for the subtype of dry eye - aqueous, evaporative or mixed - that is being treated.
References
1. Walsh K, Jones L. The use of preservatives in dry eye drops. Clin Ophthalmol. 2019;13:1409-25.
2. Baudouin C, Labbe A, Liang H, et al. Preservatives in eyedrops: the good, the bad and the ugly. Prog Retin Eye Res 2010;29:312-34.
3. Pisella PJ, Pouliquen P, Baudouin C. Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. The Brit J Ophthalmol 2002;86:418-23.
4. Jaenen N, Baudouin C, Pouliquen P, et al. Ocular symptoms and signs with preserved and preservative-free glaucoma medications. Eur J Ophthalmol 2007;17:341-9.
5. Januleviciene I, Derkac I, Grybauskiene L, et al. Effects of preservative-free tafluprost on tear film osmolarity, tolerability, and intraocular pressure in previously treated patients with open-angle glaucoma. Clin Ophthal (Auckland, NZ) 2012;6:103-9.
6. Clouzeau C, Godefroy D, Riancho L, et al. Hyperosmolarity potentiates toxic effects of benzalkonium chloride on conjunctival epithelial cells in vitro. Mol Vis 2012;18:851-63.
7. Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma 2008;17:350-5.
8. Yalvac IS, Gedikoglu G, Karagoz Y, et al. Effects of antiglaucoma drugs on ocular surface. Acta Ophthalmol (Scand) 1995;73:246-8.
9. Noecker RJ, Herrygers LA, Anwaruddin R. Corneal and conjunctival changes caused by commonly used glaucoma medications. Cornea 2004;23:490-6.
10. Kahook MY, Noecker R. Quantitative analysis of conjunctival goblet cells after chronic application of topical drops. Adv Ther 2008;25:743-51.
11. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf 2017;15:276-83.
12. Jones L, Downie LE, Korb D, et al. TFOS DEWS II Management and Therapy Report. The ocular surface 2017;15:575-628.
13. Rolando M, Crider JY, Kahook MY. Ophthalmic preservatives: focus on polyquaternium-1. Expert Opin Drug Deliv 2011;8:1425-38.
14. Choy CK, Cho P, Boost MV. Cytotoxicity and effects on metabolism of contact lens care solutions on human corneal epithelium cells. Clin Exp Optom 2012;95:198-206.
15. Labbe A, Pauly A, Liang H, et al. Comparison of toxicological profiles of benzalkonium chloride and polyquaternium-1: an experimental study. J Ocul Pharmacol Ther 2006;22:267-78.
16. Brignole-Baudouin F, Riancho L, Liang H, et al. Comparative in vitro toxicology study of travoprost polyquad-preserved, travoprost BAK-preserved, and latanoprost BAK-preserved ophthalmic solutions on human conjunctival epithelial cells. Curr Eye Res 2011;36:979-88.
17. Marsovszky L, Resch MD, Visontai Z, et al. Confocal microscopy of epithelial and langerhans cells of the cornea in patients using travoprost drops containing two different preservatives. Pathol Oncol Res 2014;20:741-6.
18. Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf 2017;15:511-38.
19. Nasser L, Rozycka M, Gomez Rendon G, et al. Real-life results of switching from preserved to preservative-free artificial tears containing hyaluronate in patients with dry eye disease. Clin Ophthalmol 2018;12:1519-25.
20. Bron A, Chiambaretta F, Pouliquen P, et al. [Efficacy and safety of substituting a twice-daily regimen of timolol with a single daily instillation of nonpreserved beta-blocker in patients with chronic glaucoma or ocular hypertension]. J Fr Ophtalmol 2003;26:668-74.
21. Goldberg I, Graham SL, Crowston JG, et al. Clinical audit examining the impact of benzalkonium chloride-free anti-glaucoma medications on patients with symptoms of ocular surface disease. Clin Exp Ophthalmol 2015;43:214-20.
22. Uusitalo H, Egorov E, Kaarniranta K, et al. Benefits of switching from latanoprost to preservative-free tafluprost eye drops: a meta-analysis of two Phase IIIb clinical trials. Clin Ophthalmol 2016;10:445-54.
23. Campagna P, Macri A, Rolando M, et al. Chronic topical eye preservative-free beta-blocker therapy effect on the ocular surface in glaucomatous patients. Acta Ophthalmol Scand Suppl 1997:53.
24. Kahook MY, Noecker RJ. Comparison of corneal and conjunctival changes after dosing of travoprost preserved with sofZia, latanoprost with 0.02% benzalkonium chloride, and preservative-free artificial tears. Cornea 2008;27:339-43.
25. El Hajj Moussa WG, Farhat RG, Nehme JC, et al. Comparison of Efficacy and Ocular Surface Disease Index Score between Bimatoprost, Latanoprost, Travoprost, and Tafluprost in Glaucoma Patients. J Ophthalmol 2018;2018:1319628.
26. Lee HJ, Jun RM, Cho MS, et al. Comparison of the ocular surface changes following the use of two different prostaglandin F2alpha analogues containing benzalkonium chloride or polyquad in rabbit eyes. Cutan Ocul Toxicol 2015;34:195-202.
27. Lopez Bernal D, Ubels JL. Quantitative evaluation of the corneal epithelial barrier: effect of artificial tears and preservatives. Curr Eye Res 1991;10:645-56.
28. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea 2012;31:472-8.
Optometrist Karen Walsh is the professional education team leader and a clinical scientist at the Centre for Ocular Research & Education (CORE), based at the University of Waterloo, Canada. She has previously worked in the contact lens industry and in clinical practice in the UK and is a fellow of the International Association of Contact Lens Educators and the British Contact Lens Association.