AUSCRS 2018: The most successful ever
This year’s Australasian Society of Cataract and Refractive Surgery (AUSCRS) meeting was held in Noosa, Queensland from October 17-20.
It was the most successful and well attended in the 22-year history of AUSCRS. Over 400 registered, including doctors, technical and administration staff and industry representatives. There was also a reasonable attendance from New Zealanders this year, although there were far more South Islanders than North Islanders again. The exception to this was Dr Dean Corbett who has become a regular, major contributor to our only major local cataract and refractive surgery meeting of the year. The high numbers this year appeared to be bolstered by an increase in the number of younger ophthalmologists and trainees attending. This year, we also had the highest number of invited overseas speakers to date.
This overall theme of this year’s meeting was Ride the Wave, in keeping with the location. Every session also had its own individual and unique theme, with presenters dressed by AUSCRS organisers in different costumes appropriate to the theme of their session.
Monofocal vs multifocal IOLs
One of the highlights of AUSCRS is the Gold Medal Lecture and this year’s lecturer was Professor Thomas Kohnen, Department of Ophthalmology chair at Goethe University in Frankfurt. He gave an excellent talk on Presbyopia Correcting IOLs: Current Options and Solutions to Problems, beginning with a discussion on the published results of monovision with monofocal IOLs. He defined the current approach to monovision as targeting a refraction of between -1.00D and -1.50D in the near vision eye, referencing AUSCRS president Professor Graham Barrett’s paper that showed about one quarter achieved spectacle independence. Kohnen also discussed accommodating IOLs and said no currently available accommodative IOL has proved accommodative ability and that not everyone who reads with an accommodating IOL accommodates.
He then moved onto multifocal IOLs, basing his discussion on his own experience dating back to the late 1980s and the original 3M diffractive bifocal IOL, and overviewing Alcon’s ReSTOR diffractive bifocal IOL, noting the main problem with all diffractive refractive multifocal IOLs were halos, starburst and glare. Nonetheless, published studies show much higher rates of spectacle independence with multifocal IOLs than with monovision, about 85% compared to 25% with monovision. Many studies show 92-95% of patients would chose a multifocal IOL again, he said.
In 2011, he began using trifocal diffractive IOLs from both Physiol FineVision and Zeiss. He soon stopped using bifocal IOLs as his patients were happier with vision for all distances. He noted that the Oculentis low add MF20 and MF15 IOLs had a lower rate of spectacle independence than trifocal IOLs, as did extended-depth-of-focus (EDoF) IOLs such as the J&J Symfony. The AcuFocus small aperture IOL was a useful option in post radial keratotomy patients, he added.
When it comes to success with trifocals, the indication for using a trifocal IOL has to be right, he continued, with the patient having the correct motivation of achieving spectacle independence while understanding the potential side effects of the lens. Other points for success included:
- Dry eye must be treated first
- EDoF IOLs are a better choice if there is any corneal irregularity
- Centration and size of the capsulorhexis are important
- Achieving emmetropia is very important including using all the newest IOL formulae such as Barrett, Olsen and Hill
- Corneal astigmatism must be treated well. Kohnen uses 35% toric trifocal IOLs and digital marking
Complications, EDoF IOLs and laser presbyopia treatment
The next session focused on surgical complications and included cases of trauma after cataract surgery, management of dense posterior subcapsular cataracts, radial tears with femtosecond laser anterior capsulotomy and small posterior capsule rents.
The take home message from the following session covering the results of EDoF and trifocal IOLs surgery was that while modern EDoF IOLs can cause night-time halos when driving, the issues with night driving were less marked and easier to adapt to than trifocal IOLs. The downside of EDoF IOLs was that unaided near vision is not as good as with the trifocal IOLs.
This session finished with one of the most interesting papers of AUSCRS. Professor Sunil Shah from the UK’s Birmingham and Midland Eye Centre talked about a novel scleral microperforation laser treatment designed to treat presbyopia using scleral relaxation. He discussed both the traditional Helmholtz theory of accommodation and the more recent, less widely accepted theory from Schachar. Hardening of both the crystalline lens and the sclera both happen with ageing. The treatment involves using an Erbium YAG laser to make multiple micropores in the sclera in four quadrants, about 4mm posterior to the limbus, with each treatment lasting 14 seconds. Early results show improved, uncorrected distance vision in low hyperopes as well as improved, unaided intermediate and near vision. Problems with the treatment at present include making the holes too deep. OCT guidance may be a future refinement. The intraocular pressure also drops via increasing uveoscleral outflow.
Cataract surgery, dry eye, SMILE and CXL
There were a number of highlights during the second day too. Sydney-based Associate Professor Michael Lawless gave a very good paper on assessment of dry eye in cataract and refractive surgery patients using both validated questionnaires and tear film osmolarity measurements. He concluded that about 60% of patients presenting for corneal refractive surgery or refractive cataract surgery require some tear film optimisation. Most can be improved using a course of topical steroids but Meibomian gland dysfunction treatments are also useful.
Dr Anil Anora spoke about his experience with SMILE, presenting data giving a worldwide ectasia rate of 1 in 100,000 after 1.5 million procedures. In my own opinion, an ectasia rate for SMILE is still difficult to quantify as some of my own LASIK patients have presented with mild cases of ectasia over 10 years post-operatively. Certainly, one of the driving factors towards increasing use of SMILE versus LASIK is the possibility of the improvement in long-term corneal mechanical strength but only time with tell us.
Miami-based Dr William Trattler’s talks included a number of highlights, such as a case of post-LASIK keratectasia in a 70-year-old that then progressed over the next decade of his life and a 75-year-old with progressive keratoconus. Trattler shared his approach to epithelium-on corneal collagen cross linking with riboflavin (CXL) and why he finds it just as effective in his practice as epithelium-off CXL.
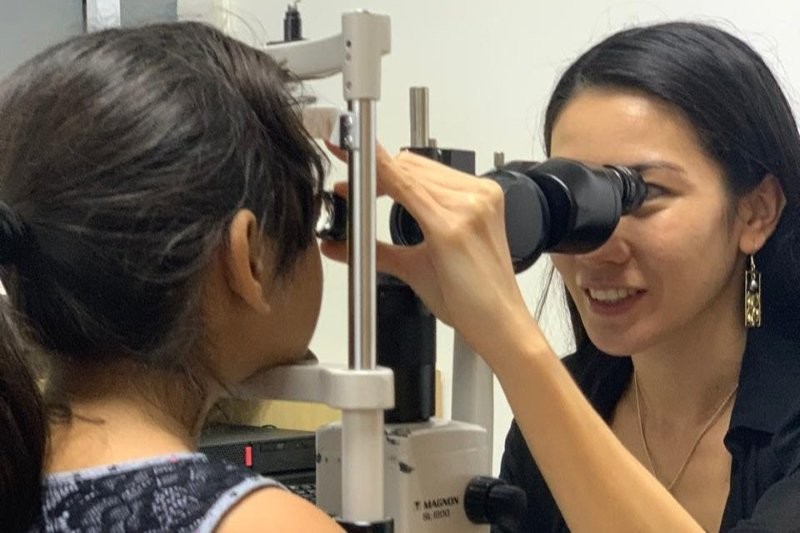
What to wear? CSMO and MIGS
The third and final day began with an interesting and entertaining session on patient-doctor communication using role play between different cataract surgeons and other conference attendees, who played some very interesting patients! There was discussion about what cataract surgeons wear for consultations, with some saying they wear surgical scrubs. Very few Australian ophthalmologists now wear a tie when consulting.
Another highlight of the final day was Prof Kohnen’s talk on the European multicentre trial on the prevention of cystoid macular oedema (CSMO) after cataract surgery in non-diabetics, the ESCRS PREMED study. This large, prospective, randomised study showed that patients treated with a combination of topical bromfenac 0.09% and dexamethasone 0.1% had a lower risk for developing CSMO after cataract surgery than patients treated with a single drug. Kohnen noted the most effective treatment for CSMO is sub-conjunctival triamcinolone. Melbourne-based Dr Lewis Levitz then presented a literature review on the efficacy of NSAID eye drops on the prevention of CSMO, concluding that to prevent one case of CSMO about 300 patients needed to be treated.
The take home message from the MIGS for glaucoma session was that some devices have too high long-term complication rates and the safest procedures were Schlemm’s canal-based surgeries. Dean Corbett compared two of these, the iStent and Hydrus, and found at two years there was a similar IOP drop.
AUSCRS 2019 is coming to New Zealand
Next year’s AUSCRS meeting will be held in Queentown, New Zealand from July 17-20. It would be great to see a much-improved turnout from New Zealand anterior segment surgeons, particularly from the North Island. It is important we support our local ophthalmology meetings, especially as next year’s AUSCRS will be returning to our own country.
I look forward to seeing many more of my colleagues attending what is not only an excellent scientific meeting, but without doubt one of the most entertaining ophthalmology meetings of the year.
Dr David Kent is a consultant ophthalmologist with Fendalton Eye Clinic and Christchurch Eye Surgery. He is a member of both the American and Australasian Societies of Cataract and Refractive Surgery and the New Zealand AUSCRS council representative.