Aussie malpractice attempted murder case sparks safety review
Australian medical governance bodies have welcomed the application of “the full force of the law”, following the conviction of a medical practitioner for the attempted murder of a pharmacist after she reported his suspected misconduct. In a joint statement, the Medical and Pharmacy Boards of Australia and the Australian Health Practitioner Regulation Agency (AHPRA) also say they are committed to ensuring the confidentiality and safety of notifiers and have initiated an independent review of their policies and procedures.
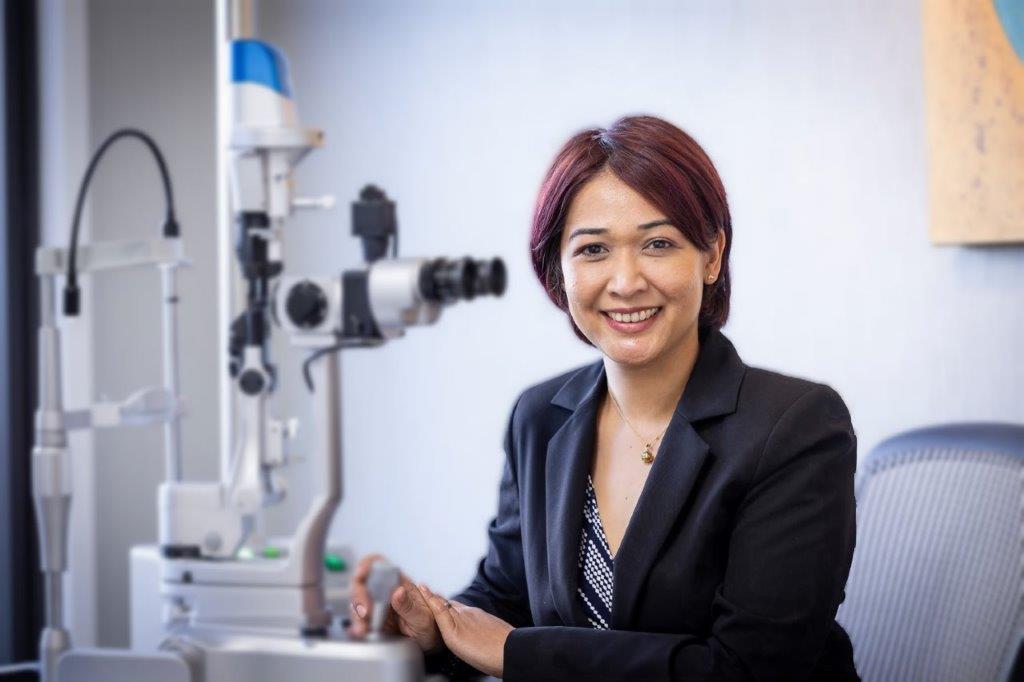
Adelaide GP Brian Holder, 69, was earlier this month found guilty of attempted murder of Port Lincoln pharmacist Kelly Akehurst and jailed for 16 years. Ms Akehurst agreed to her name being disclosed to the doctor when reporting him for alleged misconduct after his scripts for high quantities of diazepam, oxazepam and panadeine forte attracted her attention. The Medical Board of Australia had subsequently placed conditions on Dr Holder’s registration relating to his ability to prescribe Schedule 4 medicines.
On 10 October 2017, Dr Holder had driven to the pharmacy, lured the pharmacist out from behind the counter with a bunch of flowers and tried to stab her with a 15-centimetre fishing knife. Ms Akehurst suffered deep lacerations on her arms and hand while defending herself with the help of a customer.
Media reports say court documents reveal Ms Akehurst was told by AHPRA that if she was prepared for her name to be disclosed with her report, the referral would be expedited and “carry more weight”.
In their statement, the Medical and Pharmacy Boards of Australia and the Australian Health Practitioner Regulation Agency (AHPRA) say they have been shocked and appalled by the case. They add they have a legal obligation to ensure their processes are fair and transparent to both the individual making the complaint and the registered health practitioner about whom the concern has been raised.
For the vast majority of notifications, they say, people agree to be identified so a practitioner can respond to a complaint: “This is our preference because it provides everyone involved in the complaint the relevant information and supports an open and fair process. Our ability to do our job well depends on people telling us about their concerns. We want everyone to be safe when reporting to us for the greater good.”
The organisations have asked independent ombudsman and Privacy Commissioner, Richelle McCausland, to review their policies and procedures in relation to safeguarding the confidentiality of notifiers and any additional steps that can be taken. They have also confirmed the review will begin immediately and the findings will be published.
“We will continue to do as much as we are able, as regulators of individual health practitioners, to ensure we protect the public from potential harm,” they say in their statement. “We want it to be safe for people to report their concerns and will continue to review our policies and processes in light of relevant findings, including this latest case.”