BEBs, zebras and lots of SMILES
The first Eye Institute seminar of 2019 was hosted by Dr Nick Mantell, who introduced the surgery’s new marketing advisor, Janelle Brunton-Rennie, who’s worked with Dr Mantell in the past.
With a new marketing team in place, it was no surprise to see a new venue - the swish Sofitel in Auckland’s Viaduct Harbour - and a new format, including some great nibbles and a slightly longer programme. The mid-May, new Friday night timing was also a drawcard as the venue was packed to capacity, requiring an overflow room for some attendees who were able to watch the presentations on a large screen, while enjoying their wines.
BEB, ophthalmology myths and OCTs
Eye Institute patriarch, Dr Peter Ring kicked off proceedings with a look at benign essential blepharospasm (BEB), a neuropathological disorder characterised by abnormal blinking or spasms of the eyelids.
More common in women than men, symptoms can be caused by several factors including the environment and stress and can become so bad a patient can’t read, watch television, drive or walk, leading to anxiety and depression. Longer term outcomes include eyelid and brow ptosis, dermatochalasis, entropion and canthal tendon abnormalities and it should not be confused with keratoconjunctivitis sicca, Bell’s palsy, eyelid myokymia or hemifacial spasm, said Dr Ring, adding a family history of dystonia for blepharospasm will aid diagnosis. Treating BEB includes rest, support groups and sunglasses to help with photophobia, and dry eye disease treatments as this is often associated with BEB. Medicines aren’t particularly effective, however, as the central control centre is unknown, said Dr Ring, though anti-anxiety drugs can be helpful in some cases.
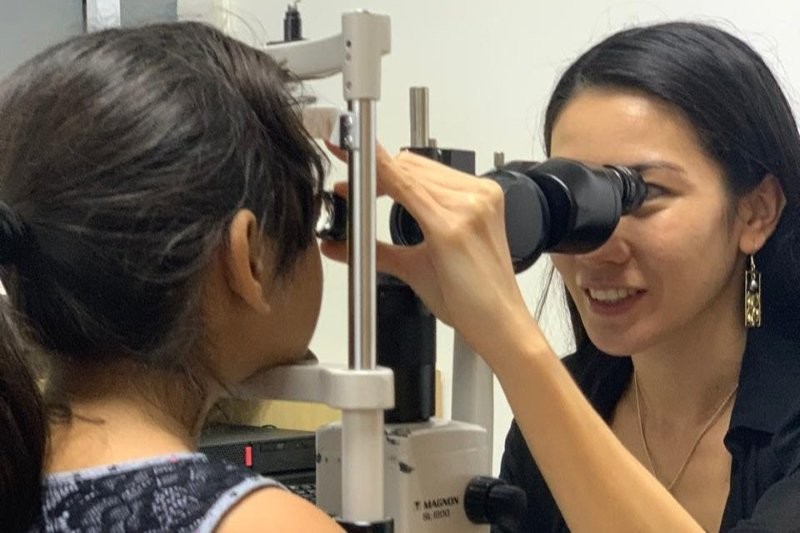
Dr Divya Perumal then provided a very practical presentation on interpreting optical coherence tomography (OCT) for glaucoma, stressing how different OCTs can lead to different results, before Dr Simon Dean busted a few myths relating to ophthalmology and oculoplastics.
The body’s healing response is normally six weeks, but remodelling takes three to six months, said Dr Dean. Steroids do have a place in the healing process but must be used warily as they can block the body’s own inflammatory healing response and not treat the cause of the inflammation. “My mantra is only use steroids when they work in a week.” He also questioned the use of drops for dry eye disease as they can mask the symptoms and provide false hope, he said. “If the deficiency is the lipid layer, why replace the aqueous layer?”
Zebras not horses
Dr Narme Deva reviewed paraneoplastic retinopathies that result from cancer somewhere in the body, not the local presence of cancer cells, can occur before, during or after a cancer diagnosis and can result in a “devastating loss of vision”.
The two that affect the eye are: CAR, carcinoma-associated retinopathy, which almost always precedes a cancer diagnosis and typically results in rapid, progressive vision loss, often with photopsias and a ring scotoma; and MAR, melanoma-associated retinopathy, which is usually associated with an existing melanoma diagnosis and results in a sudden onset of photopsias and nyctalopia, without much visual acuity or colour impairment.
“If you don’t suspect zebras, then you can’t look beyond the eye, which is important as the patient might come to you first!” Said Dr Deva.
Corneoplastics, more steroids and not POAG
After a refreshment break, Dr Adam Watson tackled corneoplastics, where the ocular surface and eyelids are treated as one functional unit, a discipline that developed quickly in the UK during and after WWII treating wounded soldiers with facial burns.
Dr Ben LaHood, then took a controversial (and amusing) stance promoting topical steroids and discussing his preferred treatment plans for different anterior segment conditions. If used and monitored carefully, steroids can be used to speed up recovery and provide quick relief to the patient for contact lens overwear, marginal keratitis, blepharitis, pterygia and post-viral keratitis, he said.
Diagnosing when primary open angle glaucoma (POAG) is not POAG can be a tricky business, continued Dr Graham Reeves, illustrating his point with a number of interesting case studies. These included patients with pseudoexfoliative glaucoma, neovascular glaucoma, traumatic glaucoma and uveitic glaucoma. Non-POAG is common, he said, stressing the importance of taking a good history, knowing the patient’s ethnicity and doing a thorough examination, including gonioscopy, to diagnose POAG or not.
Thumbs up for SMILE and HSV
Dr Mantell returned to the podium to share Eye Institute’s own experience and research into SMILE and how it compares with LASIK today. He concluded there’s now been enough testing to demonstrate SMILE’s benefits and its place in the refractive surgeon’s armamentarium. “We’ve really benefitted from all the people who have gone before us enabling us to develop the best procedures. We now consider it a safe procedure… and see dry eye less often with SMILE.”
Bringing the evening to a close Dr Jay Meyer tackled herpes simplex virus (HSV) which can have multiple presentations in the eye, making it challenging to diagnose and treat.
Eye Institute’s next Auckland seminar will be held on Tuesday 20 August from 5.30pm to 9pm at the Four Points Sheraton Hotel.