Cataract surgery and dry eye
Cataract surgery is one of the most common elective surgical procedures performed worldwide. Advancements with surgical instrumentation and lens implant technology have made it increasingly popular as a treatment for both visual rehabilitation and refractive correction. Patient expectations have never been higher, and superb results with rapid recovery are readily achievable. Sounds great, right, so what’s the problem? “My eyes are constantly irritated… they were never like that before the surgery, doctor!”
Unfortunately, dry eye disease (DED), while frequently dismissed as a minor annoyance following cataract surgery, can be a significant cause of patient dissatisfaction, visual symptoms and poor surgical outcomes. Preoperatively, accurate biometric measurements require an optimal ocular surface state. Furthermore, the numerous presbyopia-correcting IOL options that are becoming increasingly popular, are notoriously unforgiving with regard to visual quality in the presence of a suboptimal ocular surface.
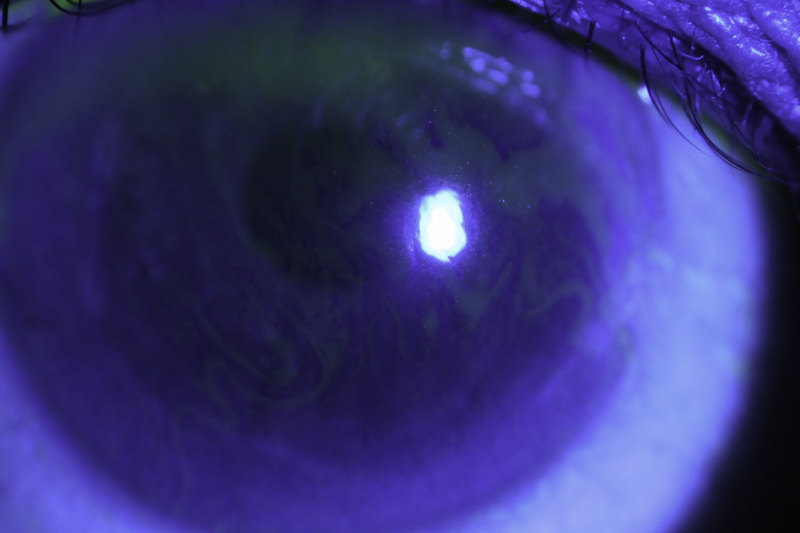
The prevalence of ocular surface signs in the patient demographic that undergoes cataract surgery is extremely high. In the PHACO study, 77% of patients had corneal staining preoperatively. Although, many of these patients may be asymptomatic, disruption of the delicate homeostasis of the tear film and ocular surface can lead to manifestation of symptoms which then become frustratingly difficult to manage reliably, despite the significant advances in our understanding of DED and its treatment options. Several studies have indicated that patient symptoms and signs are negatively influenced by cataract surgery and some may take up to six months to recover.
The TFOS DEWS II report represents an extensive body of work led by world experts in dry eye, and their recently published iatrogenic dry eye report presents a comprehensive literature review which includes cataract surgery. There is no question that many interventions involved in cataract surgery are responsible for post-operative DED. The most likely perpetrators are topical medications (and their preservatives) used pre- and post-operatively, oxygen free radicals and pro-inflammatory cytokines generated in response to surgical trauma, and the corneal incisions which invariably sever corneal nerves. Similar, though more extensive, corneal nerve injury is well described following LASIK surgery where postoperative dry eye is one of the chief sources of postoperative dissatisfaction. Light toxicity from the operating microscope has also been implicated. Diabetic patients in particular seem to be more at risk of iatrogenic DED.
Therefore, a comprehensive dry eye evaluation should be performed for all prospective cataract surgery patients. Pre-operative recognition and optimisation of DED signs and symptoms is a critically important factor in managing such patients. Ideally this should begin at the point of referral, when surgery is being considered. The TFOS DEWS II reports are an ideal source for up-to-date diagnosis and management recommendations.
Avoiding topical preservatives in at-risk patients, minimising postoperative drop toxicity and actively managing dry eye symptoms with topical lubricants where necessary are simple measures that can help post-operatively.
On the horizon, “dropless cataract surgery” (where intraocular slow-release preparations of steroid and antibiotic are used instead of topical post-operative medications) may be a useful step forward in preventing DED in cataract surgery patients. Stay tuned!
Laser refractive surgeons recognised all of this long ago and consider it standard care to treat dry eye pre- and post-operatively. We should all adopt the same standard of care for our cataract patients.
References
Epitropolous AT et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cat Refract Surg 41(8):1672-7.
Trattler WB et al. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017; 7(11):1423-30.
Cochener B et al. Prevalence of meibomian gland dysfunction at the time of cataract surgery. J Cataract Refract Surg. 2018 Feb;44(2):144-148
Xue W et al. Long-term impact of dry eye symptoms on vision-related quality of life after phacoemulsification surgery. Int Ophthalmol. 2018 Feb 1. doi: 10.1007/s10792-018-0828-z. [Epub ahead of print]
Gomes JAP et al. TFOS DEWS II iatrogenic report. The Ocular Surface (2017) 15(3):511-38.
Dr Stuart Carroll is a consultant ophthalmologist at Auckland Eye and Greenlane Clinical Centre in New Zealand with specialist knowledge in cataract and refractive surgery, strabismus and paediatric ophthalmology.