Covid-19: Considering our more vulnerable patients
Optometry has been one of the hardest hit industries in the Covid-19 era. Not being an essential service, yet at the same time being a health provider, with a high patient-to-practitioner risk of SARS-CoV-2 transmission and no way of changing to a contactless business, is a cocktail of anxiety. Balancing the financial implications with the health risks of reopening would leave even the most accomplished juggler with bruises. But, however stressed and battered we feel about the need to get back to normal business quickly, many of our patients are also struggling with this new normal.
As large chunks of society revel at breaking loose from their bubbles to hit the local takeaway, an equally large proportion see the emergence from their enforced security into this strange new world as less than comfortable. I am referring to the ‘over 70s’.
Suddenly the over 70s have become a homogenous group with a label that forces them to confront their own vulnerabilities - physical and mental, as well as financial. The media hammers them with “our most vulnerable/fragile/at risk group who need to be protected”, when many are still working and used to being the dependable ones who care for others. Some have had their confidence shaken, while others are feistily fighting back at having their freedom brutally curtailed with declarations of independence and tales of how they have survived worse.
For the majority though, venturing out of lockdown is a very anxious time as the initial Level 4 restricted bubble felt far more secure than the broken bubble they now face. The doctor, dentist and optometrist are some of the scariest places to go when exiting the bubble, because those are places where sick people go. For those whose bubbles may contain immunosuppressed people, such as those undergoing or recovering from cancer treatment or other health issues, the added responsibility and anxiety is intense.
Many are also anxious that healthcare treatment delays may have been detrimental to their health, exacerbating conditions and weaknesses that were already present. Long delays in hospital waiting lists, now extended by the virus taking priority, have been at best frustrating and at worst terrifying for some.
Years of education drummed into them about early detection and the risks of missing appointments may drive some to consider their need to be more urgent than anyone else’s, making them attempt to elbow others out of the way. Hopefully these will be the vocal minority, but the point is patients have different priorities and stresses and need careful management by skilled empathetic staff who recognize this.
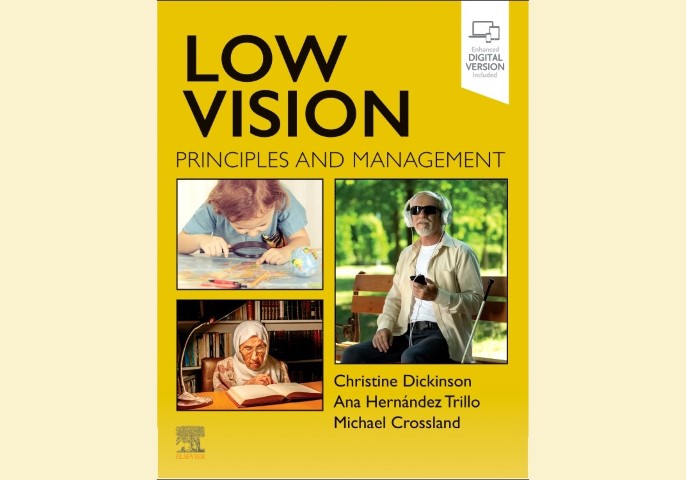
There is no doubt that many businesses have been forced to adopt new ways of doing business, with some finding efficiency improvements in these changes. For some, however, particularly those without technology or the knowledge to use it, this adds challenges and frustrations, particularly if they also suffer from low vision. Answerphones which direct people to go online for appointment assessments or to find more information are a barrier to some people, forcing them to look for help elsewhere.
Contactless payment has come into its own during lockdown. Touching money and grubby keypads are now considered a dire source of contagion, but many elderly people are not ready for click and collect. Some still struggle with remembering pin numbers or seeing the well-worn keypads, a situation often made worse by being presented with EFTPOS machines at nose level on high counters.
Then there’s the added burden of financial stress. We all know about that, but so do our patients. Confronted with being classified as high risk and fragile, our over 70s may also be struggling with the reality of living with much reduced superannuation payments as the returns from their investments dwindle.
Our more vulnerable patients’ anxieties need to be acknowledged and dealt with, preferably by reassurance from staff as soon as they contact or enter a practice. Even something as simple as seeing their optometrist in full personal protective equipment, while it may be the new norm for us, may create anxiety. Don’t assume a sign on the door or at the reception desk has been seen, read or understood, but do assume they need our help, because most of them will.
Naomi Meltzer has worked in optometry for more than 30 years. She runs an independent optometry practice specialising in low vision consultancy in Auckland.