Diabetes, dry eye and ‘Substance P’?
Diabetes has now reached epidemic proportions affecting millions of people across the world. It is estimated around 54% of patients with diabetes suffer from some degree of dry eye syndrome.
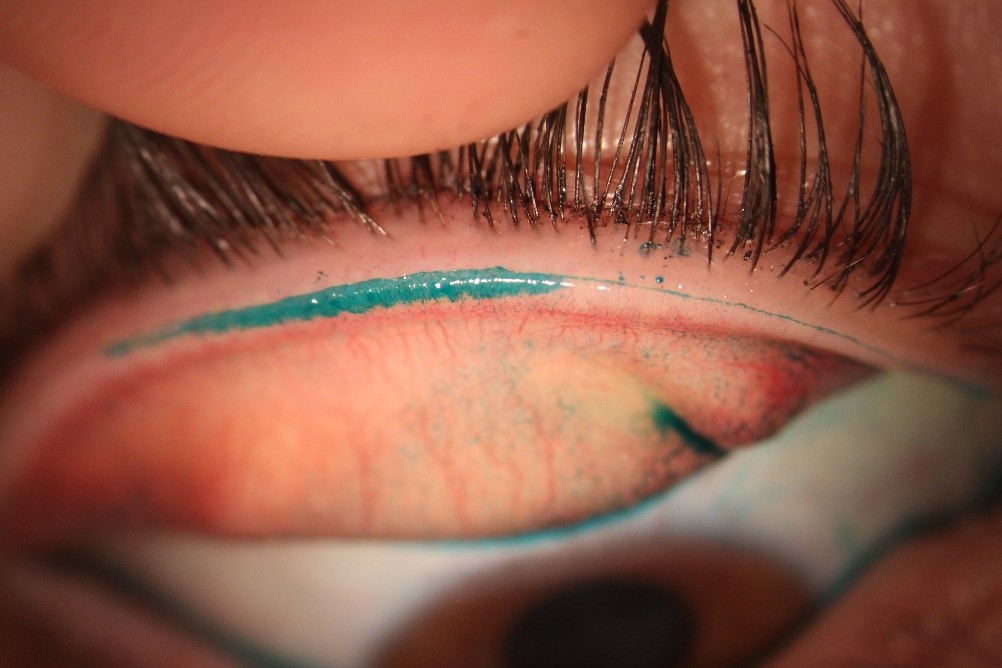
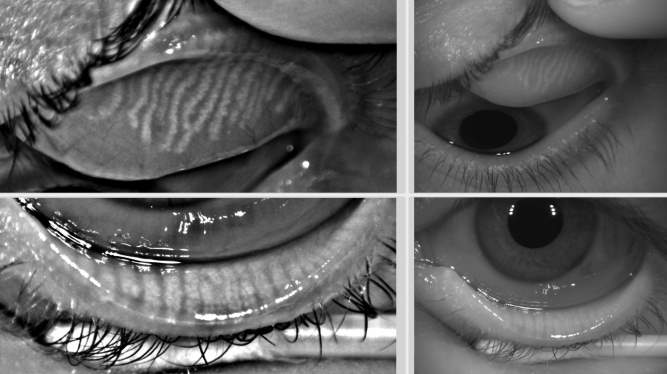
Patients with diabetes commonly complain of burning and foreign body sensation in their eyes. In severe cases, this may result in reduced corneal sensitivity, aberrant wound healing ability of the cornea, increased risk of infection and the eventual development of diabetic neurotrophic keratopathy. Interestingly, there is growing evidence of the involvement of neurotransmitters in the tear film offering an interesting potential pathway for future ocular surface treatment strategies.
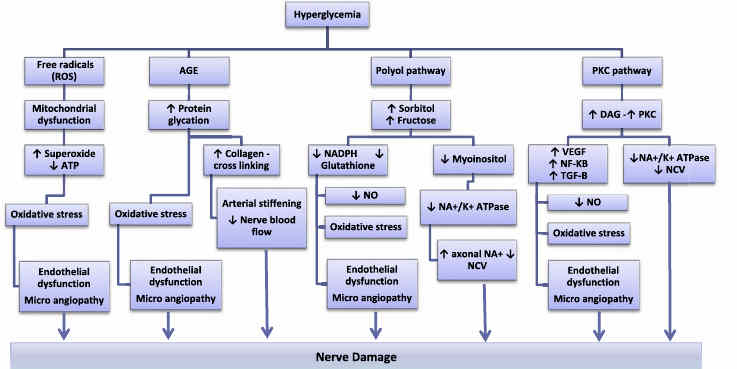
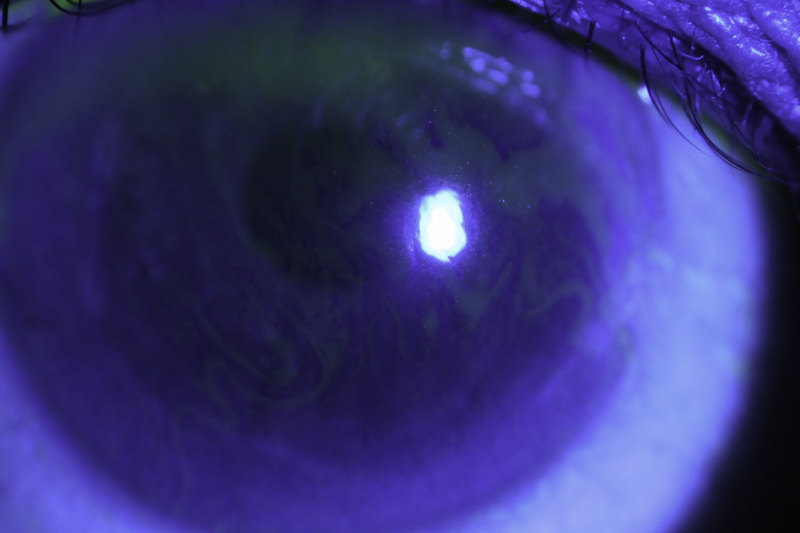
Chronic hyperglycaemia, diabetic peripheral neuropathy, decreased insulin levels, microvasculopathy and systemic hyperosmotic disturbances are the most common risk factors for diabetes mellitus associated dry eye syndrome (DMDES). Insulin is critical for proliferation of the acinar lacrimal gland and corneal epithelial cells, whereas hyperglycaemia induces significant histological changes in the lacrimal gland. This suggests a strong role of oxidative stress in dry eye syndrome. A number of factors, however, are responsible for ocular surface changes in patients with diabetes which ultimately may lead to corneal nerve damage (fig 1).
Substance P is a neuropeptide released from the trigeminal nerve endings located in the cornea, lacrimal gland and conjunctiva. In isolation and with other hormones (including neuropeptide Y, gene-related peptide, insulin-like growth factor 1 and vasoactive-intestinal peptide) substance P plays a crucial role in wound healing while providing maintenance and nutrition to the cornea by promoting the migration, proliferation and differentiation of corneal epithelial cells. In diabetes, substance P levels decrease, contributing to poorer wound healing and increased susceptibility to corneal neurotrophic ulcers, due to decreased epithelial migration. This finding has been confirmed in a recent pilot study by Markoulli et al (see p38). which compared patients with diabetes to a healthy control group. Substance P also decreases in spinal fluid and the peripheral nervous system which plays an important role in causing diabetic peripheral neuropathy. Evidently, diclofenac decreases the levels of Substance P in the tear film, something one might want to take into account when using Voltaren eye drops in patients with diabetes. Substance P and insulin growth factor-1, however, reportedly show good efficacy in healing neurotrophic diabetic keratopathy, but these treatment options are yet to be completely explored.
Where to from here
A number of studies focusing on neurotransmitters and their potential role in treating diabetes-associated dry eye are underway or planned. As well as focusing on diabetic retinopathy, the leading cause of blindness in diabetes, significant attention needs to be paid to DMDES in clinical practice as it can have a severe effect on quality of life. The pathogenesis of DMDES, however, remains elusive and further clinical trials are warranted and ongoing by different research groups in the UK, Australia and also Auckland.
We will certainly have more to report on this interesting topic in next year’s review of dry eye research in the region.
References
Manaviat MR, Rashidi M, Afkhami-Ardekani M, Shoja MR. Prevalence of dry eye syndrome and diabetic retinopathy in type 2 diabetic patients. BMC Ophthalmol 2008;8:10.
Alves Mde C, Carvalheira JB, Modulo CM, Rocha EM. Tear film and ocular surface changes in diabetes mellitus. Arq Bras Oftalmol 2008;71:96-103.
Nishida T, Inui M, Nomizu M. Peptide therapies for ocular surface disturbances based on fibronectin–integrin interactions. Progress in retinal and eye research 2015;47:38-63.
Davidson HJ, Kuonen VJ. The tear film and ocular mucins. Veterinary ophthalmology 2004;7:71-77.
Markoulli M, You J, Kim J, et al. Corneal nerve morphology and tear film substance P in diabetes. Optometry and Vision Science 2017;94:726-731.
Marfurt CF, Echtenkamp SF. The effect of diabetes on neuropeptide content in the rat cornea and iris. Investigative ophthalmology & visual science 1995;36:1100-1106.
Yamada M, Ogata M, Kawai M, Mochizuki H, Mashima Y. Topical diclofenac sodium decreases the substance P content of tears. Archives of Ophthalmology 2002;120:51-54.
Dr James Slater is a clinical research fellow in the New Zealand National Eye Centre at the University of Auckland, where he is focusing on corneal nerves and diabetes. Dr Stuti Misra is a lecturer and researcher at the University’s Department of Ophthalmology. Her research focus includes ocular surface abnormalities and corneal imaging.