Eye Institute: identifying dangers
Eye Institute’s May seminar was a busy, collegial affair with many Auckland-based optometrists making the most of the delicious refreshment-fuelled opportunity to catch up with colleagues and gain extra CPD points. By Lesley Springall
Dangerous floaters
Dr Peter Hadden kicked-off proceedings with an interesting and somewhat worrying look at floaters. If new floaters are associated with visual loss or the presence of blood or ‘tobacco dust’ in the eye, it’s likely the patient has a retinal tear, which can lead to a retinal detachment. Floaters can also indicate large cell lymphoma, uveitis and mild vitreous haemorrhage. “If there is a haemorrhagic posterior vitreous detachment, a thorough examination must be undertaken. If the haemorrhage obscures a view of the peripheral retina then consider B-scan and urgent vitrectomy.” Optometrists should check floaters’ colour, size and whether they are anterior or all over the vitreous, and if there are other signs of disease. If your patient has a vitreous haemorrhage and reports having had a massive headache, send them to the A&E department immediately, as they could have a subarachnoid haemorrhage, stressed Dr Hadden.
Serum, CDR’s usefulness and photopsia
Dr Nick Mantell provided a novel take on the subject of the moment, dry eye, discussing the latest research suggesting serum eye drops may provide some significant relief and support to the ocular surface and the tear film. Attempts to isolate specific tear film proteins to treat ocular surface disease have had limited success, but serum drops have been shown to maintain both epithelial cells and keratocytes better than artificial tears, and speed up epithelial cells’ healing, showing they could be a good treatment for dry eye.
Dr Graham Reeves asked whether cup-to-disc ratio (CDR) is as important as it’s made out to be; a concern driven by several factors including its prevalence in the US where doctors are required and paid to record it. In his experience, CDR is an inadequate way of assessing glaucomatous cupping. “We need to retrain ourselves to think about the neuro-retinal rim width,” he said.
Dr Will Cunningham took to the podium to discuss flashes, photopsia and photosphenes and how to discern what are normal or abnormal flashings. A good place to start is to ask if it’s in one eye or both eyes, as one eye is likely to mean it’s local, while two eyes could mean it’s brain-related and thus more worrying. As with all things, taking a detailed patient history and clinical examination is crucial. There are many causes of unilateral photopsia, including toxoplasmosis, birdshot chorioretinopathy (birdshot uveitis), acute macular neuroretinopathy, multiple sclerosis and choroidal tumours. While bilateral photopsia can be caused by ischaemia or oedema, medications, such as digitalis or anti-depressants, and hereditary or autoimmune retinopathies. The most common causes, however, are posterior vitreous detachments, retinal tears and migraines, he said.
Corneal erosions, yellow spots and allergies
Dr Adam Watson provided an upbeat presentation on recurrent corneal erosions, explaining how he enjoys treating them which is why, perhaps, he seems to attract so many of them. Normally these are caused by past trauma, epithelial basement membrane dystrophy or past photorefractive keratectomy (PRK). At first, they should be treated with antibiotic prophylaxis and pain relief, perhaps a bandage contact lens, and then hopefully stabilised with a combination of oral doxycycline and topical corticosteroids. If that doesn’t work, burring and then phototherapeutic keratectomy (PTK), if all other treatments have failed.
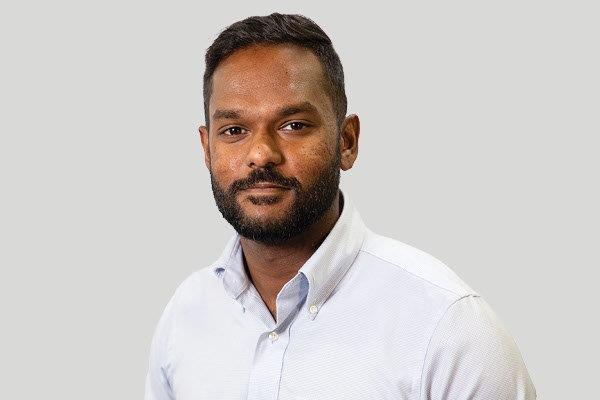
Eye Institute’s newest recruit, Dr Narme Deva then tackled the tricky issue of yellow spots, linking back to her colleagues’ talks on floaters and flashes. Again, taking a comprehensive patient medical history is key. In the clinical exam, look for adjacent structures and symmetry, isolate the site of pathology, use multimodal imaging, and if any vision loss, blind spots or inflammation is detected, or if they are in a vision-threatening location, refer them quickly, she said.
Dr Simon Dean discussed the good, the bad and the ugly in ocular allergy. The good, like allergic conjunctivitis, is easy to treat; the bad, vernal and atopic conjunctivitis, are harder to treat; while the ugly, giant papillary conjunctivitis and contact dermatitis, look bad, but are easier to treat. Vernal and atopic keratoconjunctivitis account for less than 5% of all ocular allergies and can be treated with tacrolimus as a substitute for steroid treatments. In a nutshell, “If it’s itchy, it’s allergy”, he said.
EI’s community trust and low vision
The final speaker of the day, Dr Shanu Subbiah, reminded the audience that at some point everyone struggles with their vision and that low vision is not just debilitating in itself, but causes falls, reduced self-care, depression and anxiety, and a large financial burden on society. Surgery can be considered, he said, for example, the Scharioth IOL provides greater magnification at a reduced reading distance and can be implanted in patients with advanced maculopathy and pseudophakes. But all eye care professionals should help their low vision patients by helping to increase contrast by improving their light sources; reducing glare by adjusting light sources and providing filters; enlarging images by encouraging them to use magnifiers and other technical aids; and referring them to low vision specialists, something, he admitted, many ophthalmologists are not particularly good at. At the end of the day, “low vision, is useable vision,” he said.
Earlier in the evening, Dr Subbiah also officially launched and discussed Eye Institute’s new community trust. The charitable initiative is designed to support families who don’t quite qualify for the Community Services Card, by funding up to 400 eye examinations and providing subsidies up to $250 towards glasses.
For more on the Eye Institute’s new trust, see NZ Optics’ May issue or visit http://www.eyeonoptics.co.nz/articles/archive/eye-institute-s-new-community-trust/