FDA warns against Raindrop inlay
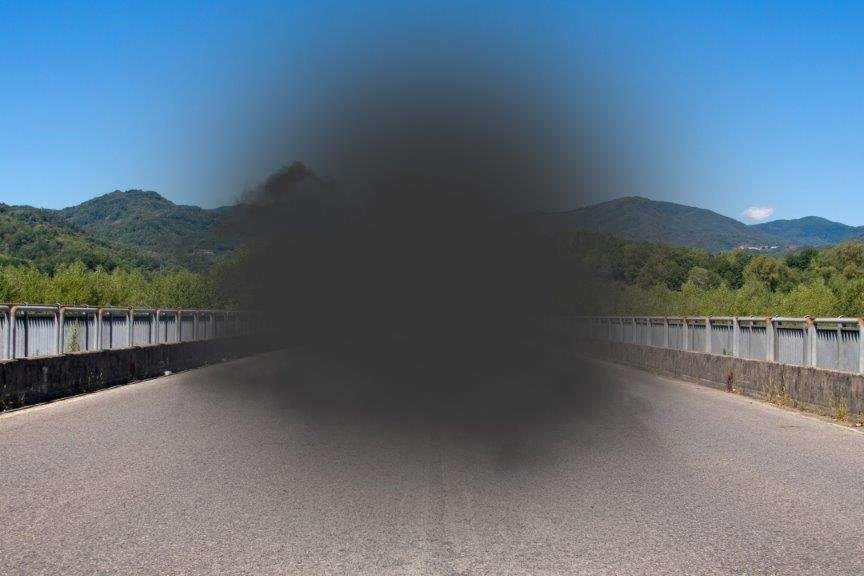
The US Federal Drug Administration (FDA) has issued a safety communication warning eye care providers and patients about the Raindrop Near Vision Inlay after follow-up studies showed three quarters of patients developed corneal haze.
The FDA approved the device in 2016, but has now withdrawn that approval and is working with Optics Medical to recall all remaining stock of the inlay. It urges those already implanted with the device to keep regular appointments with their eye care provider and seek evaluation sooner if they develop any new or bothersome symptoms. The patient’s physician, it says, will determine appropriate treatment options based on the results of an evaluation.
The FDA’s approval of the Raindrop Near Vision Inlay device in 2016 was supported by a prospective, non-randomized clinical study in patients who had the device implanted. As a condition of approval, FDA mandated that the sponsor perform a post-approval study (PAS) designed to follow patients enrolled in the original study at least through five years after surgery. The most recent interim data showed the rate of central corneal haze, at any time during the study, was 42%, the presence of haze at any location within the cornea was 75% and 22 patients developed their first episode of haze 60 months after the device was implanted. The percentage of patients with two or more lines’ loss on the eye chart caused by corneal haze was greater than what was observed during the original clinical study.
Of the 150 patients enrolled in the PAS, 20.7% were treated with steroid eye drops at any time during this study and 23.7% who still had the device implanted were prescribed steroid eye drops for corneal haze. In some cases, the steroid eye drops did not make the haze go away, and the device had to be removed.
Of the 150 patients enrolled in the PAS, 35 patients to date have had their device removed either during the post-approval study or after they left the original clinical study. Of these, 31% had the device removed due to corneal haze, and 28% due to unresolved inflammation (which may include additional cases of haze). One patient first developed haze six months after removal of the device. In addition, some patients continued to have corneal haze even after the device was removed. This study is ongoing and patient follow-up is continuing.