Glaucoma and IOP, Xen and nocturnal blood pressure
Efficacy, safety and risk factors for failure of Xen Gel Microstent implantation versus standalone trabeculectomy
Schlenker MB, Gulamhusein H, Hengerer IC et al
Ophthalmology 2017;124:1579-1588
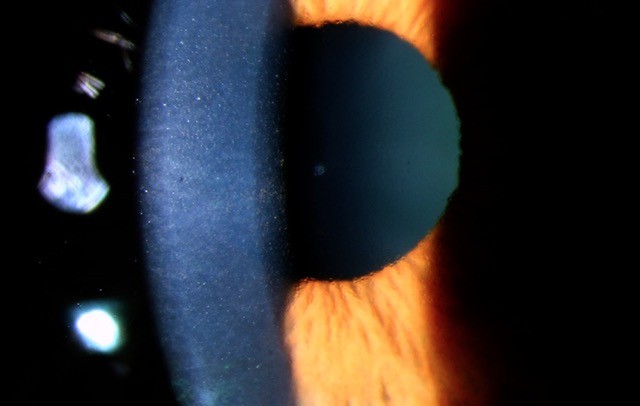
The Xen gel stent is a new procedure that has recently become available in New Zealand and is considered an alternative option to trabeculectomy. The purpose of this study was to evaluate the efficacy, safety and risk factors for failure of Xen versus trabeculectomy. An international multicentre retrospective interventional cohort study was performed. Patients had open angle glaucoma and uncontrolled IOP despite maximum medical therapy, and no previous surgery.
There were 354 eyes of 293 patients included in the study. The primary outcome measure was the failure rate between the two groups - defined as an IOP of <6 mmHg or >17 mmHg without glaucoma medication at least one month after surgery. The study also looked at ‘qualified success’ defined as an IOP between 6 and 21 mmHg with medication.
No significant difference in failure rate between the two procedures was identified (Hazards ratio 1.2, 95% CI 0.7-2.0). This was also the case for qualified success (HR 1.3, CI 0.6-2.8). The time to 25% failure was also not significantly different between the groups. Diabetes was the only factor significantly associated with failure, while Caucasian ethnicity was associated with a decreased risk of failure. Complications were mostly transient, occuring in 9% of Xen and 16% of trab patients. Post op. interventions such as bleb needling were common, occuring in 43% of Xen and 31% of trab patients.
Comment
The proposed advantages of Xen include reduced surgical time, reduced risk of complications and more rapid visual recovery. This study suggests both procedures are similar in their efficacy over the duration of this study and the safety profile is also similar although there was a slightly lower rate of complications for Xen. Further randomised clinical trials are, however, needed as well as studies to evaluate the cost-effectiveness of Xen versus trabeculectomy.
Glaucomatous optic neuropathy associated with nocturnal dip in blood pressure
Melgarejo JD, Lee HJ, Petitto M, et al
Ophthalmology 2018 (in press)
The purpose of this study was to determine if noctural blood pressure (BP) is associated with an increased risk of glaucoma. An observational cross-sectional study was performed involving a subset of participants from the Maracaibo Aging Study. These participants had to be at least 40 years of age, and had measurements including OCT, visual field (VF) testing, IOP <22 mmHg, and 24-hour blood pressure monitoring. Glaucomatous optic neuropathy (GON) was based on the presence of optic nerve damage and VF defects.
There were 93 subjects included in the study with a mean age of 61.9 years and 87% were female. Of 185 eyes evaluated, 27% had signs of GON. The primary finding was that these subjects with GON had significantly lower 24 hour and nocturnal diastolic BP levels than those participants without GON. However, multivariate analysis indicated that the glaucoma damage was not related to average systolic or diastolic BP levels over 24 hours, during the day or at night time. Instead, extreme decreases (>20% compared to daytime BP) in night time systolic and diastolic BP was identified as the significant risk factor for glaucomatous damage (odds ratio 19.8 and 5.5 respectively).
Hence the results of this study suggest that the link between nocturnal BP and GON is due to extreme dipping in BP rather than low nocturnal BP levels alone.
Comment
The results of this study support the hypothesis that significant nocturnal dips in BP are a risk factor for glaucoma. Hence individuals at risk of nocturnal dips in BP do need to be assessed and monitored for glaucoma. Timing of antihypertensive intake to avoid nocturnal dips would also be advised. Patients already diagnosed with normal-tension glaucoma and who are progressing, may need to undergo 24-hour BP monitoring to determine if nocturnal dips in BP is a contributing factor.
Variation in IOP and the risk of developing OAG: The Los Angeles Latino Eye Study
Jiang X, Torres M, Varma R
American Journal of Ophthalmology 2018 (in Press)
The purpose of this study was to determine whether measures of intraocular pressure (IOP) variation are independently associated with the risk of developing open angle glaucoma (OAG). This was part of a population-based, longitudinal study involving 3666 individuals with no history of OAG at baseline and followed up four years later.
Maximum IOP, standard deviation (SD) of IOP, range of IOP and mean IOP were derived from participants after taking several measurements at multiple visits. OAG diagnosis was based on the consensus of experts who had access to all clinical examination data (including stereoscopic fundus images and visual field testing). Multivariate logistic regression analysis was also performed.
The incidence of OAG occurred in 73 study participants over the four years. The three measures of IOP variation (maximum IOP, SD and range of IOP) were all identified to be independently associated with the risk of developing OAG. This was still the case when participants were separated into those with a mean IOP of less than 15 mmHg and those with 15 mmHg or higher. Mean IOP was associated with OAG risk only in those with higher IOPs and not in those with lower IOPs. Maximum IOP was identified to be the most significant predictor of OAG.
Comment
This study suggests that variations in IOP and in particular maximum IOP are damaging to the optic nerve and are independent risk factors for glaucoma. This highlights the value of measuring IOP variation (with day phasing or the water drinking test) as part of the work up of glaucoma suspects. This may also be useful in patients with glaucoma progression as it is likely IOP variation also plays a role here.
About the author
Dr Hussain Patel specialises in glaucoma and cataract surgery and is a consultant ophthalmologist at Greenlane Clinical Centre, Auckland District Health Board and a senior lecturer in ophthalmology at the University of Auckland. He also works in private practice at Eye Surgery Associates, Auckland, and Hamilton Eye Clinic.