Glaucoma: beta blockers, optic disk size and OCT
Systemic medication associations with presumed advanced or uncontrolled POAG
Zheng W, Dryja TP, Wei Z et al
Ophthalmology 2018 (article in press)
Review
The purpose of this study was to identify associations between systemic medications and primary open angle glaucoma (POAG) using a database study. A total of 6,130 POAG cases were included and matched to 30,650 controls by age and gender. Participant prescription drug use was analysed over a five-year period and multivariate logistic regression analysis was used to identify associations between both individual drugs and drug classes. There were 1,763 drugs and 423 drug classes studied.
The most significant finding was that selective serotonin reuptake inhibitors (SSRIs), used to treat depression, were strongly associated with a reduced risk of POAG, with citalopram the most significant drug in this class. SSRI users were at 30% less risk of developing POAG versus non-users.
The drug class beta-blockers showed the second most significant protective association. This included orally administered beta-blockers only, as patients on topical beta-blockers were excluded.
In contrast, calcium channel blockers (used to treat hypertension) were strongly associated with an increased risk of POAG, with amlodipine the most significant drug in this class. There were other associations identified but these failed to reach significance after multivariate analysis.
Comment
The protective association for beta-blockers is to be expected given the IOP-lowering effect they provide. The potential relationship between SSRIs (protective) and calcium channel blockers (increased risk) with POAG are less expected and could point towards new drug associations. However, further research is needed to confirm these findings and to understand the role of serotonin metabolism and calcium channels in glaucoma.
A small disc area is a risk factor for visual field progression in POAG: The Glaucoma Stereo Analysis Study
Kitaoka Y, Tanito M, Yoloyama Y, et al
Journal of Ophthalmology 2018 (article in press)
Review
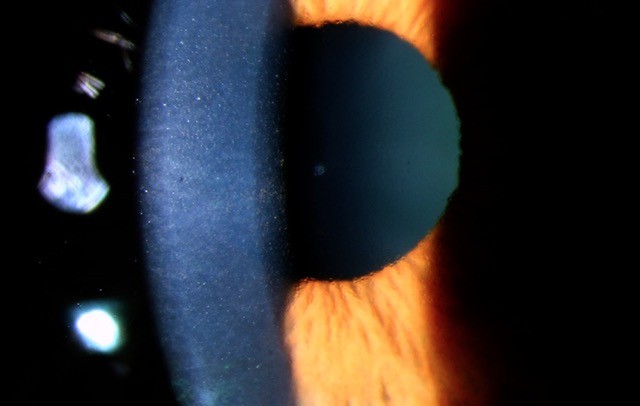
This cross-sectional multicentre collaborative study used a stereo fundus camera to assess various morphological parameters of the optic nerve head (ONH) in glaucoma patients. The study included a total of 187 eyes of 187 patients with POAG or normal tension glaucoma (NTG). Researchers separated the patients into two groups – those with visual field progression (MD slope <−0.3 dB/year) and those without (≧−0.3 dB/year). Within each group they then determined if there were any associated ONH parameters.
Optic disc parameters analysed included the vertical disc diameter, disc area, cup area and cup volume. ONH morphological parameters were calculated with prototype analysis software. The correlations between glaucomatous visual field progression and patient characteristics for each ONH parameter were analysed with Spearman’s rank correlation coefficient.
After logistic regression analysis was performed, small disc area was identified as the parameter most significantly associated with visual field progression in this study. The odds ratio was calculated to be 0.49/mm2 disc area, indicating that if the disc area increased by 1mm², the probability of progression would decrease by about half. This also means that if the disc area decreased by 1mm², the probability of progression would be approximately twofold greater.
Comment
This study suggests that glaucoma patients with small optic discs (disc area <1.6mm² or vertical disc height of <1.2mm) are more at risk of glaucoma progression than those patients with average or large optic discs, and hence need to be more carefully monitored for the development of glaucoma progression.
Use of optical coherence tomography by non-expert personnel as a screening approach for glaucoma
Liu M, Cho C, Quigley H et al
Journal of Glaucoma 2018, Vol 27, Issue 1, p64-70
Review
This pilot study was conducted to assess optical coherence tomography (OCT) as a screening tool for glaucoma when used by non-expert personnel. A prospective case control study was performed including 54 patients with open angle glaucoma and 54 age-matched controls. Optovue iVue SD-OCT imaging was performed by non-professional photographers (who underwent <30 min of training) on undilated patients.
The vertical cup-to-disc ratio measured by iVue had the highest sensitivity (0.96 at 90% specificity) for detecting glaucoma out of all the parameters measured. More than 95% of those with glaucoma were identified versus 7% without glaucoma. The iVue cup-to-disc measurements and sensitivity/specificity were also highly correlated to clinician grading (experts using stereo-ophthalmoscopy) that was performed as part of the study.
Several retinal nerve fibre layer parameters, especially inferior quadrant thickness, also had impressive sensitivity and specificity results with respect to identifying glaucoma. However, ganglion cell complex measurements did not perform well.
Comment
This study demonstrates the potential role OCT has as a community-based screening tool for glaucoma. Furthermore, the screening could be performed by lay personnel with minimal training and on undilated patients. Further studies are needed however to confirm the above findings and to further evaluate OCT as a glaucoma screening tool.
About the author:
Dr Hussain Patel specialises in glaucoma and cataract surgery. He is a consultant ophthalmologist at Greenlane Clinical Centre, Auckland District Health Board, and a senior lecturer in ophthalmology at the University of Auckland. He also works in private practice at Eye Surgery Associates, Auckland, and Hamilton Eye Clinic.