Glaucoma, steroids, OSSN and more
Eye Doctors’ last Grand Round of 2018 was introduced with a warm reminder about the importance of eye health by Dr Andrew Riley who shared a video of Volunteer Ophthalmic Services Overseas’ (VOSO’s) latest trip to Tonga. The video paid tribute to the local people, many of whom had travelled great distances to visit the team, and the team itself, which consisted of Dr Riley, optometrists Kylie Dreaver and John Tarbutt, Queensland ophthalmologist Dr John-Paul Blanc and Pacific Eye Institute-trained Dr Duke Mataka and his locally-based team.*
Moving on to meatier topics, Dr Riley then kicked off the seminar proper, tackling the thorny issue of steroid use and its effect on intraocular pressure (IOP). Any age group can be affected, but those most at risk include children under 10 and older people; those with suspected or identified glaucoma; high myopes and diabetics. The eye pressure rise is usually identifiable within three weeks, however it can be hours or even years, though it should normalise within four weeks of stopping the steroid. Management includes halting steroid use or steroid sparing agents; using fluomethalone 0.1% as it has less effect on IOP; laser trabeculoplasty; or intraocular steroids, such as Ozurdex. The latter which has been much in the news both for its apparent efficacy and a recent batch recall, is a new biodegradable intravitreal implant containing 700μg dexamethasone. This is very potent, said Dr Riley, so the patient only requires tiny amounts, making its effects on IOP far less than other steroids.
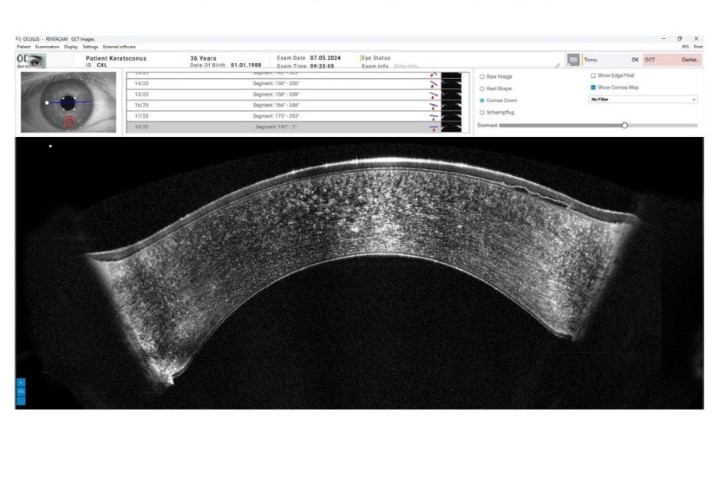
Dr Penny McAllum tackled ocular surface squamous neoplasia (OSSN), an abnormal proliferation of atypical squamous epithelial cells on the ocular surface causing a broad spectrum of disease. Its epidemiology varies greatly with little incidence in the UK (0.2 cases per million people per year) to Australia (19) and Uganda (35), and it has a high correlation with HIV. Here and in Australia, it is primarily associated with men who work outdoors, such as farmers. It is often picked up in routine eye checks where patients complain of redness, irritation and/or blurred vision or have a noticeable lump. The most important assessment is whether the neoplasia is invasive or not, ie. it has breached the basement membrane and moved into the underlying stroma. “OCT or impression cytology may be helpful, but a biopsy is required to confirm the diagnosis,” said Dr McAllum. “But with anything that looks a bit suspicious around the limbus, suspect OSSN.” Once diagnosis is confirmed, use surgery and topical antimetabolite chemotherapy, which reduces recurrence to 5% at one year and 12% at five years.
Dr Mark Donaldson, who had flown in from Chicago’s American Academy of Ophthalmology meeting that morning, then delivered a very practical presentation, sharing case studies and discussing abnormalities in OCT scans when measuring retinal nerve fibre layer (RNFL) thickness to diagnose glaucoma. The technology of OCTs differ and results can be affected by dry eye and post-subcapsular cataract. Also you must expect some thinning of the RNFL as patients get older (about 1μm a year), but if the reduction is matched with field defects, then the results are far more significant, he said.
Dr Andrew Riley closed the last Grand Round with a paediatric-focused talk, paying tribute to one of Eye Doctors’ founding partners, Dr Shuan Dai who has been lured across the ditch to become director of ophthalmology at Children’s Health Queensland and Lady Cilento Children’s Hospital in Brisbane.
Stepping into his role temporarily, until Dr Julia Escardo-Paton takes over the paediatric mantel this year, Dr Riley stressed the importance of listening to parents when they tell you something is wrong with their baby’s sight. He discussed the difference of pseudo-strabismus and strabismus – “a wide nasal bridge and epicanthal fold can cause the illusion of crossed eyes in kids” – and strabismus treatments and emergencies, including the sudden onset of esotropia and exotropia. He also touched briefly on leukocoria or white pupillary reflex, which can indicate cataract, retinal detachment, retinopathy of prematurity, retinal malformation, intraocular infection (endophthalmitis), retinal vascular abnormality and intraocular tumour. Finally, on a more sombre note, Dr Riley stressed that a retinal haemorrhage with unknown aetiology is highly suggestive of a non-accidental incident (NAI). If you suspect this, talk to the family’s GP and/or report it to the NAI team at Greenlane. You can save a child’s life, he said.
*Full story at www.nzoptics.co.nz/articles/archive/voso-helps-out-in-tonga/