Glaucoma
Risk factors for rapid glaucoma disease progression
Chan TCW, Bala C, Siu A et al
American Journal of Ophthalmology 2017;180:151-157
The purpose of this study was to determine the intraocular and systemic risk factor differences between a group of rapid glaucoma disease progressors and non-rapid disease progresses. A retrospective case-control study was performed and included 48 rapidly progressing eyes (> 1dB mean deviation (MD)/year) and 486 non-rapid progressing eyes (progression < 1dB MD/year). Clinical and demographic data (age, sex, CCT, IOP, refraction, medications) along with medical, surgical and ocular histories were collected.
Cardiovascular disease (CVD) was identified to be a major risk factor for predicting rapid disease progression in glaucoma patients. In fact, patients with CVD were 2.3 times more likely to develop rapid progressive glaucoma compared to patients without CVD. Additionally, worse baseline MD, lower baseline IOP, more frequent ocular hypertensive medication changes, and number of IOP lowering surgeries were also significant predictors of rapid progression.
Other risk factor including lower CCT, pseudoexfoliative syndrome (PXF), disc haemorrhages, and hypotension were more common in the rapid progressor group but the effect was not statistically significant in the multivariate analysis. Interestingly, average IOP and IOP fluctuation were not significantly different between the groups. All other risk factors studied including sex, age, refraction, diabetes, migraine, vasospasm, steroid use and hypotension were not shown to be statistically significant predictors of rapid disease progression in this study.
Comment
The identification of cardiovascular disease (CVD) as a major independent predictor of rapid glaucoma progression is an important observation. It may be that CVD reflects poor blood circulation and hence fits with the “vascular theory” of glaucoma, however additional research is needed to further clarify the relationship between CVD and glaucoma progression. In the meantime, for clinicians managing glaucoma, it is important to consider each patient’s overall medical health and to work with their GP or physician to address any potential cardiovascular risk factors that can be modified to help reduce disease progression.
Virtual clinics in glaucoma care: face-to-face versus remote decision-making
Clark J, Puertas R, Kotecha A et al
British Journal of Ophthalmology 2017;101:892-895
This study aimed to evaluate the agreement between ophthalmologists’ management decisions during a face-to-face standard outpatient visit and those made in a ‘virtual clinic’.
The virtual clinic was set up within a hospital facility and was staffed by technicians and nurses. Consecutive patients that met the eligibility criteria (including open angle glaucoma and greater than six-monthly follow-ups) were included in the study (n=204). Virtual clinic patients underwent the same routine examinations and investigations that were to be conducted at their clinic appointment (visual fields, optic disc imaging etc.). A subsequent face-to-face clinical assessment was completed by a glaucoma consultant or fellow for each patient. The virtual clinic records were reviewed remotely by one of two glaucoma consultants, and 12 months later by the clinicians that had undertaken the original clinical exam. The inter-observer and intra-observer decision making of virtual vs standard care was determined.
The rate of adverse disagreement between face-to-face and virtual review was identified to be 7/204 (3.4%, 95% CI 0.9% to 5.9%) where virtual review failed to predict a need for accelerated follow-up identified in face-to-face review. These seven patients were considered ‘stable’ in the virtual clinic review but ‘unstable’ during the face-to-face assessment. Inter-observer agreement was considered only ‘fair’ but improved to ‘moderate’ when only consultant decisions were compared against each other. Intra-observer agreement was also considered ‘moderate’. The authors concluded that although virtual clinics may not provide the same level of sensitivity at detecting unstable disease as standard outpatient care, significant misclassification events are rare and no serious safety concerns were identified.
Comment
This study suggests that the use of virtual clinics in the management of stable glaucoma patients is a safe, logistically-viable option for selected patients. Patients that have a low risk of progression to significant visual loss would be most suitable, and virtual review by a consultant is the most reliable, hence virtual clinics could play an important role in the overall strategy to deal with the ever-increasing demand for glaucoma services.
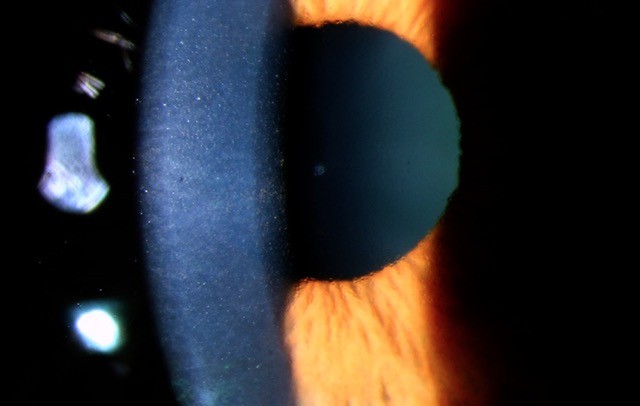
Risk of visual field progression in glaucoma patients with progressive retinal nerve fibre layer thinning
Yu M, Lin C, Weinreb RN et al
Ophthalmology 2016; 123:1201-1210
The aim of this study was to determine whether progressive retinal nerve fibre layer (RNFL) thinning is predictive of visual field (VF) loss in glaucoma. A prospective study was performed that included 139 primary open angle glaucoma patients (240 eyes) followed over more than five years. RNFL imaging and VF testing was performed at approximately four month intervals. Progressive RNFL thinning was determined by guided progression analysis (GPA) and trend-based progression analysis (TPA) using the Cirrus HD-OCT (Zeiss). VF progression was detected according to EMGT criteria and pointwise linear regression (PLR) criteria.
Progressive RNFL thinning was seen in 27% of eyes using GPA and 49% of eyes using TPA. VF progression developed in 13% of eyes using EMGT and 16% of eyes using PLR criteria over the follow-up period. Progressive RNFL thinning was strongly identified to be predictive of the subsequent development of VF progression. RNFL progression, determined by GPA, resulted in an eight-fold increase and, TPA, a three-fold increase in risk of developing VF progression based on the EMGT criteria compared with eyes without progressive RNFL thinning after controlling for baseline measurements.
Comment
This study determined that progressive RNFL thinning, as seen on OCT, is a predictor of future visual field loss and hence functional decline in glaucoma. This emphasises the importance of detecting RNFL thinning and using this information in the decision-making process to either initiate treatment or augment treatment in glaucoma patients at an earlier stage than would otherwise occur.
About the author
Dr Hussain Patel specialises in glaucoma and cataract surgery. He is a consultant ophthalmologist at Greenlane Clinical Centre and a senior lecturer in ophthalmology at the University of Auckland. He also works in private practice at Eye Surgery Associates, Auckland, and Hamilton Eye Clinic.