Insight into dry eye, drugs and macula holes
On a very stormy evening in April, Auckland Eye held its first Insight seminar of the year over dinner at Auckland’s Orakei Bay function centre.
MC for the evening was Dr Dean Corbett who welcomed the strong turnout of attendees, kept the evening upbeat and moving, and introduced the evening’s three speakers: Drs Stuart Carroll, Stephen Best and Archie McGeorge.
Dry eye developments
Dr Carroll kicked off the evening’s talks tackling recent developments in dry eye, including the main findings of the Tear Film & Ocular Surface Society’s second Dry Eye Workshop (TFOS DEWS II), which were released last year (see NZ Optics’ September 2017 issue). He encouraged attendees to download the report, which is “lengthy but readable” or, at least, the more manageable executive summary.
As well as defining more clearly what dry eye is and what it isn’t, the report also provides some helpful recommendations for diagnosing and managing dry eye, he said. A useful tool for those wishing to offer more comprehensive service, is a free app from Allergan, the Dry Eye OSDI Questionnaire, which calculates a patient’s Ocular Surface Disease Index (OSDI) score, assessing the severity of their dry eye, said Dr Carroll. To diagnose dry eye, DEWS II recommends measuring tear osmolarity, tear film break up time, and assessing the ocular surface, the eyelids and meibomian glands. Meibography, the imaging of the meibomian glands, is particularly useful for assessing evaporative dry eye and can be performed using lid transillumination, the Oculus Keratograph and/or Tearscience’s LipiScan and LipiView. The latter being a “really good tool” to actually show patients the cause of their dry eye problems, he added.
Dry eye tests should be sequenced correctly to gain reliable results and clear explanations outlined for treatment. Many treatment options, however, have limited level 1 evidence to support their use. For example, manufacturers’ claims of superiority for many types of lubricant drops are not proven. There is evidence, however, for lipid-containing lubricant drops providing superior symptom relief for evaporative dry eye; for topical steroids reducing inflammation of the ocular surface; and that a diet rich in omega-3 foods, nuts and green vegetables helps mitigate dry eye symptoms.
Dr Carroll also outlined newer treatment options including the increasingly popular intense pulsed light (IPL) technology and Lipiflow, which have a growing evidence-base showing safety and efficacy.
Optometrists can now refer patients to Auckland Eye’s new Oasis Spa, which has been specifically designed to comprehensively diagnose and treat patients suffering from chronic dry eye disease, which includes treatment technologies such as IPL and Lipiflow.
Problems with medications
Every so often you see unusual patients where it’s unclear what’s wrong or why. With these patients its always important to take a good medical history and discuss their symptoms with colleagues, as certain medical conditions and/or medications can result in seemingly unrelated eye conditions, said Dr Best, who then went on to share some of these more unusual cases.
He also discussed some of the conundrums ophthalmologists face when treating patients on certain medications, such as anti-coagulants like warfarin or Pradaxa. Plus, many new drugs have not been used long enough by patients for us to really know all their adverse effects, he said. For example, long-term treatment with hydroxychloroquine has now been found to cause bull’s eye maculopathy.
Reactions to established drugs are normally rare, but can be serious, he added, referring to a case involving a 13-year-old boy who’d been prescribed minocycline for acne, which caused papilloedema, and another involving etidronate for osteoporosis, which is now associated with acute anterior uveitis.
Dr Best then discussed a number of other medications and their potential effects including the motion sickness patch scopolamine and central nervous system stimulants, Ritalin and cocaine, which affect the pupil; steroids which affect lens opacity and intraocular pressure; and a whole host of different drugs which adversely affect the retina and the optic nerve, including too much Viagra! Then there are those “natural” or “nutritional” remedies, many patients don’t consider to be drugs, but can have severe negative effect on eye health, such as chamomile and echinacea (conjunctivitis), St John’s wort (periocular haemorrhage) and ginko biloba (retinal haeomorrhages), he said.
“So be aware of medications and their interactions with the eye. They will occur all the time and a lot of the time you won’t even suspect them, so you need to take a good history, especially the patient’s drug history.”
Macular holes
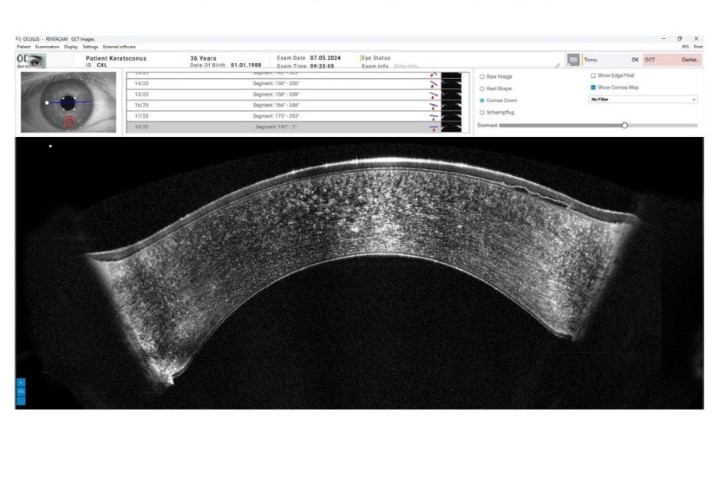
The diagnosis and treatment challenges of macular holes has become far easier since the advent of optical coherence tomography (OCT) and improved surgery tools and techniques, explained Dr McGeorge.
Idiopathic macular holes are the most common, particularly among females, over the age of 60 and patients who have a history of myopia, trauma or ocular inflammation.
They are classed as stage 1 to stage 4, with stage 4 being the most severe. Stage 1 are simply monitored as 50% can close on their own. If they progress to stage 2, however, they have a 74% chance of progressing to stage 3, making early surgical treatment the best option, he said.
In days gone by, macula hole treatments were pretty brutal, including laser treatment and vitreous surgery, which required the patient to remain face-down for two weeks. But things began to improve dramatically in the late 1990s, with the removal of the internal limiting membrane (ILM). This was followed by the introduction of better instrumentation and visualisation surgery technologies, said Dr McGeorge, including well designed forceps and “Brilliant Blue Stain”; better diagnostic and monitoring technologies, such as OCT, allowing for earlier operations; and more experienced surgeons, culminating in surgery success rates of more than 98% today, with “excellent” visual acuity results.
But a small percentage of macular holes don’t close or reopen following surgery; up to 18 months later, in some cases. The main reasons for holes reopening are epiretinal membranes, cystoid macular oedema, cataract extraction or trauma, he said.