Introducing the KinD21 project
“…should we institute collagen cross-linking on a routine basis, which would eliminate the need for multiple examinations under anaesthesia, anaesthesia for surgery and anaesthesia for suture removal, as well as anaesthesia for the follow up treatment of a corneal transplant…?” 1
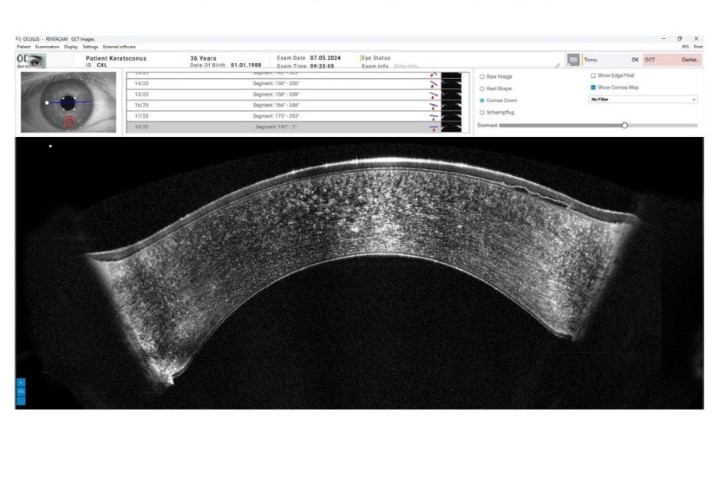
This question was raised in an invited commentary to a multi-centre study which identified that keratoconus may affect 71% of individuals with Down syndrome2. To the best of our knowledge, this is the highest estimate to date and is among the first of its kind to utilise Scheimpflug corneal imaging.
Keratoconus is a chronic, progressive disease of the cornea characterised by thinning, biomechanical weakness and corneal protrusion. It is thought to affect 0.05% of the general population. Advanced stages, which require intervention by corneal transplantation may be avoided through early treatment with corneal collagen cross-linking. Early treatment may be achieved through early detection, which is particularly important among groups at risk of keratoconus development, such as patients with Down syndrome.
Down syndrome is caused by a full or partial trisomy of chromosome 21. Studies indicate that individuals with Down syndrome have risk factors including steeper, thinner and biomechanically weaker corneas compared to the general population. Additionally, studies suggest corneal hydrops is more common in people with Down syndrome than the general population with keratoconus.
A pilot study by our team at the Special Olympics, detected keratoconus in approximately one-third of athletes with Down syndrome. To address the need for early detection and treatment in this vulnerable group, we are launching the KinD21 project: a large, population-based screening and treatment initiative for keratoconus in Down syndrome.
In this proposed project, we seek to provide eye examinations and comprehensive corneal assessments to 400 individuals with Down syndrome. This will include assessments of corneal tomography and anterior segment optical coherence tomography (OCT).
Participants diagnosed with keratoconus will be monitored at three to six-month intervals over 12 months. Individuals with progressive keratoconus will be referred for corneal collagen cross-linking. Those without keratoconus progression will be referred to an optometrist or ophthalmologist to be monitored for progression long term.
A multi-disciplinary team consisting of ophthalmologists, anaesthetists, paediatricians and participant representatives will optimise current corneal collagen cross-linking protocols. The outcomes of treatment will be observed closely over the medium-term.
Through early detection and timely treatment, we aim to reduce keratoconus-related visual impairment in Down syndrome so that the best possible visual outcomes may be achieved.
This project is supported by the Auckland Medical Research Foundation Doctoral Scholarship, a Save Sight Society grant, the Joan Ready Ophthalmology Fund, the CNJ & JJ McGhee Ophthalmology Futures Fund and a Heather Mackintosh grant.
References
- Binder PS. Topography and Tomography Findings in Patients with Down Syndrome. JAMA ophthalmology. 2018 Jun 21.
- Alio JL, Vega-Estrada A, Sanz P, Osman AA, Kamal AM, Mamoon A, Soliman H. Corneal Morphologic Characteristics in Patients with Down Syndrome. JAMA ophthalmology. 2018 Jun 21.
The KinD21 co-investigator team consists of Joyce Mathan, Dr Samantha Simkin, Dr Akilesh Gokul and Professors Dipika Patel and Charles McGhee from the University of Auckland