IOLs and MGD in Wellington
Johnson & Johnson Vision hosted a continuing education evening in Wellington to discuss Meibomian gland dysfunction (MGD) treatment and the Tecnis Symfony Intraocular lens (IOL). It was open to ophthalmologists, nurses and optometrists and it was great to see a mix of these professions in the room.
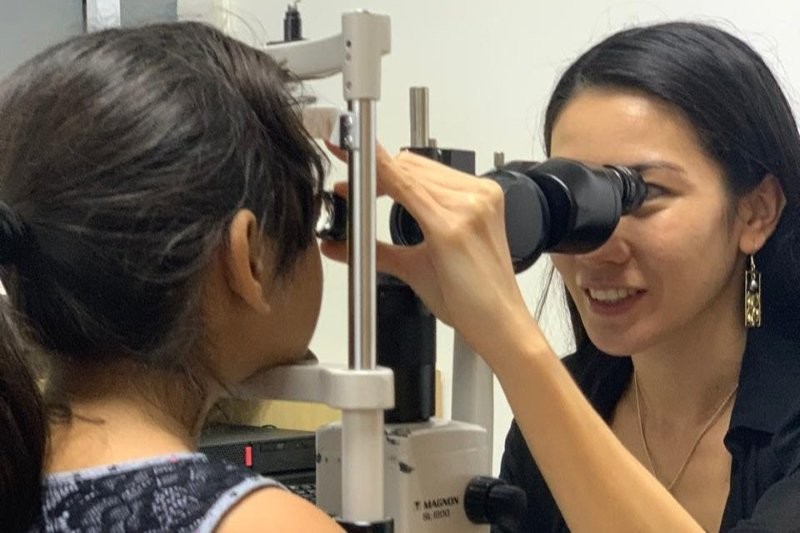
Surekha Parag, an optometrist from the Oasis dry eye spa at Auckland Eye, started the evening discussing MGD and the new treatments offered by the LipiView and LipiFlow machines. Thanks to the TFOS DEWS II report we are all aware of the important role Meibomian glands play in tear film stability. The LipiView Ocular Surface Interferometer measures lipid layer thickness (LLT) and images Meibomian gland structure to show the state of a person’s Meibomian glands, while the LipiFlow Thermal Pulsation System uses both heat and pressure to provide a good expression of the glands.
J&J’s research has shown that patients who have already lost 67% of their Meibomian glands are unlikely to notice a benefit from the LipiFlow treatment but those in the mild to moderate category, with only a third of glands lost, benefit from a single treatment, albeit after one month.
Many of the optometrists and ophthalmic nurses in attendance had their glands imaged and a couple were lucky to be treated. Personally, I love the concept of the LipiFlow but I’m not sure I am ready to let go of the perverse joy of manual gland expression just yet, though the oil collected in the unit following a treatment was quite a sight.
Dr Frank Howes, a refractive and cataract ophthalmologist from Queensland, then shared the impressive results he’s had with the Tecnis Symfony IOL. An extended-depth of focus (EDoF) IOL, the Symfony is a diffractive lens with a wave front aspheric anterior surface, allowing a balance between aberrations, range of focus and clarity.
Dr Howes said with specific and careful patient selection he was able to obtain some outstanding results one-month post-op with this IOL, with 100% of his selected patients able to read 6/6 and N6 or better unaided, and of those 84% were able to read N5. The secret to success of the Symfony, like most IOLs, is accurate measurements. This means treating dry eyes, contact lens removal for the appropriate amount of time, performing more than one astigmatic measurement and accurate IOL location in the capsule during surgery.
The key take home message was patient counselling and what to expect up to six-months post-op. Prominent flare and rings in the early stages settle relatively quickly within a month, even more within three months and again more so by the six-month post-op mark, he said. Another interesting point discussed was the concept of mini-monovision. Allowing a -0.50 distance RX in the second eye will aid the spectacle-free result.
Whilst multifocal contact lens designs are inherently different, I believe the future patient base for cataract surgery will be far better equipped to deal with the ‘simultaneous’ vision needed for great results. For the optometrists present it was great to learn a little more about the IOLs our patients might end up with.