IPE cysts, VFs and lamina cribrosa
Cysts of the iris pigment epithelium - What is new and interesting?
Jerry A. Shields, MD and Carol L. Shields, MD
Asia-Pacific Journal of Ophthalmology, Jan/Feb 2017; Vol 6, No. 1
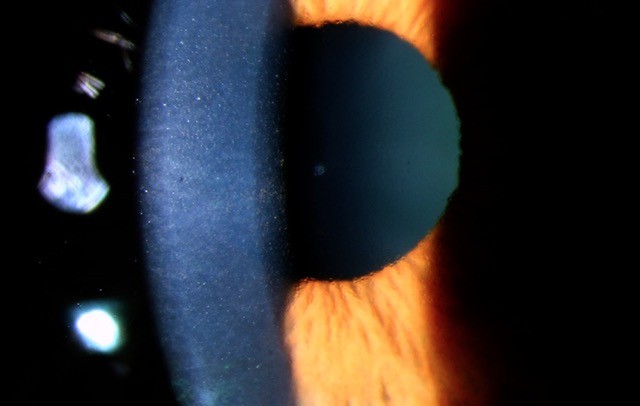
This is a very interesting article with attractive images by the shield group in the USA, in which they described the cysts of the iris pigment epithelium (IPE), not stromal ones. Lesions in 672 eyes were classified by the pupillary margin (7%), midzone (28%), peripheral (63%) or dislodged/free-floating (2%). Cysts of the IPE occurred most often in young adults (21-40 years), 34% manifesting with peripheral or mid-zonal cysts. The article also summarises the classification of IPE cysts, with descriptions of the shape of the cysts in different regions. Furthermore, the authors discuss the role of diagnostic imaging modalities, including ultrasound biomicroscopy and anterior segment optical coherence tomography (OCT), to rule out solid tumours like iris melanoma or nevi.
The most interesting part of the article is the importance of recognising iris flocculi, a bilateral multifocal variant of pupillary margin IPE cysts characterised by variable-sized dark-brown lesions that can encircle the pupil and overlie the pupillary margin. These often spontaneously collapse and then re-form, producing irregular wrinkled lesions, which can be found with dissecting thoracic aortic aneurysms, related to genetic mutation in smooth muscle of the iris and aorta. Most IPE cysts require no treatment, but those in the pupillary margin (iris flocculi) should have lifelong annual examinations for thoracic aneurysm as this could be a life-threatening condition.
Evidence-based Criteria for Assessment of Visual Field Reliability
Jithin Yohannan, Jiangxia Wang, Jamie Brown, et al
Ophthalmology 2017;124: 1612-1620
This is a retrospective study of a total of 10,262 visual fields from 1,538 eyes of 909 subjects with suspect or manifest glaucoma and ≥ 5 visual field (VF) examinations. The authors reported the impact of false-positives (FP), false-negatives (FN), fixation losses (FL), and test duration (TD) on VF reliability at different stages of glaucoma severity.
The results showed that FL had little impact on changes of MD, <0.2 decibels (dB) per 10% abnormal catch trials, and no level of FL produced ≥ 1 dB of changes MD at any disease stage. One minute increment in TD produced changes of MDs between _0.35 and _0.40 dB.
The authors proposed practical evidence-based criteria as a guide to determine VF reliability:
1. FL does not affect VF reliability meaningfully in non-naïve field takers.
2. Any level of FP decreases VF reliability, but one should be especially cautious when FPs occur in advanced disease or are found in >20% of catch trials.
3. FN has less of an impact than FP. FN does not significantly affect reliability in advanced disease unless they are high - at least 35%, but often more than this value. In early disease, FNs are more impactful, where as few as 25% FNs can have a significant impact.
4. Large increases in TD, >2-3 minutes beyond what is typical, are an indicator of poor reliability and should be taken into consideration.
In summary, this study showed that in established VF test takers, FP, FN, and TD are all clinically significant predictors of VF reliability (defined as ∆MD), with FP producing the largest impact on ∆MD and FL producing almost no impact on ∆MD.
Multiple Temporal Lamina Cribrosa Defects in Myopic Eyes with Glaucoma and Their Association with Visual Field Defects
Yu Sawada, Makoto Araie, Makoto Ishikawa, Takeshi Yoshitomi
Ophthalmology 2017;124:1600-1611
This is cross-sectional study investigating the characteristics of lamina cribrosa (LC) defects in myopic eyes. It highlights the reasons for glaucoma in myopic eyes, in particular the characteristic deformations of the parapapillary region, including optic disc tilt and torsion and parapapillary atrophy. LC is a deep component of the optic nerve and could be deformed in myopia.
In this study, Serial enhanced depth imaging OCT B-scans of the optic disc were acquired and reviewed for LC defects. The numbers and locations of LC defects and large pores in each eye were assessed, as well as the association between the locations of LC defects and VF defects. 133 eyes were assessed with open angle glaucoma OAG) and 83 eyes without OAG, with axial length of 24mm or more.
The authors found myopic eyes with OAG exhibited LC defects and large pores at similar locations as those without OAG, but in greater numbers, suggesting that these focal alternations of the LC in myopic eyes may evolve into larger defects when glaucoma develops in the eye. The number of LC defects, which was related to the optic disc tilt angle, was associated significantly with glaucomatous VF defects in both severity and location.
This suggests that myopia may influence glaucomatous VF defects through optic disc tilt by way of an increased number of LC defects at the temporal periphery.
About the author
Dr Rasha Altaie is an ophthalmologist with particular interest in pterygium surgery, paediatrics, cornea and cataracts. After training in Ireland, she received advanced clinical fellowship and sub-specialty training in cornea and anterior segment reconstruction and paediatric ophthalmology at Auckland University. She is currently working as a specialist with Counties Manukau District Health Board and at Milford Eye Clinic.