Looking under the covers
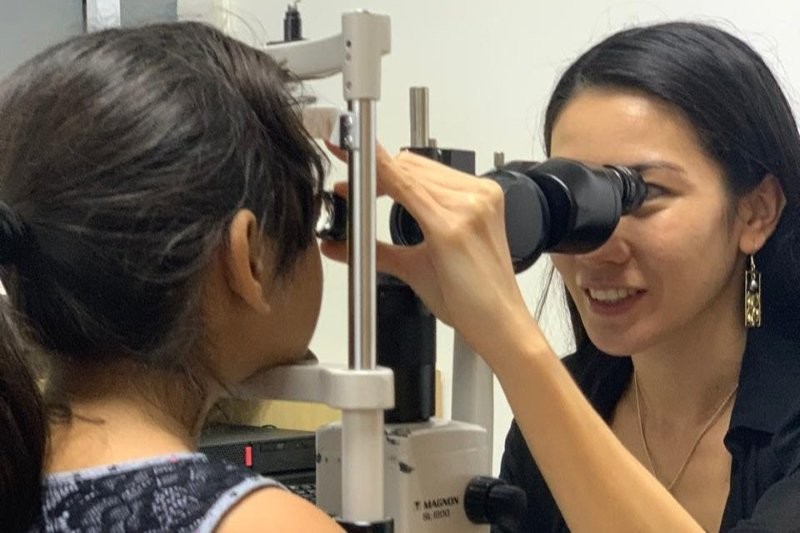
If you added a theme to Auckland Eye’s last Insight seminar, it would have to be to look under the covers. Presenters Drs Justin Mora, Jo Sims and Dean Corbett each discussed things which are not always what they seem on initial presentation, demonstrating how we need to dig deeper for clues and take thorough histories, particularly of previous or current systemic conditions, infections or inflammations.
Dr Mora tackled paediatric uveitis and glaucoma, pointing out that the most common cause of uveitis in children is usually some form of childhood arthritis and the joint problems usually appear first. Many of these children may be on steroids and therefore are at risk of developing glaucoma and cataract. Steroids are also often used to control allergic conjunctivitis. All of this may go unnoticed as children often don’t complain of pain or poor vision and children are frequently not assessed for glaucoma. But children are more susceptible to corneal oedema due to the immature endothelium being less efficient, he said, so they may present with photophobia and watery eyes due to corneal haze and have asymmetrical or deep optic nerve cupping due to damage from previous episodes.
Red flags - not just for bulls
Dr Jo Sims continued this theme, adding that 79.5% of presenting uveitis cases will have an autoimmune or autoinflammatory association; 20% will have infection as origin; and a further 0.5% will be masquerading as something else, such as lymphoma. A diagnosis of uveitis is not the endpoint but rather the start of a search and rescue mission to determine past and present history, she said, to determine what else is going on in this body?
Even when a careful history has been taken, if a compliant patient fails to make progress on treatments such as steroids, Dr Sims suggested a red flag may have been missed, so we should look elsewhere for infective, viral or other possible origins, including high-risk lifestyles or visiting high risk areas where infectious elements may be rife. Misdiagnosis or delayed diagnosis may worsen the outcome, she stressed.
Is it really glaucoma?
Dr Corbett questioned whether normal tension glaucoma (NTG) is a diagnosis or an indication of an eye with a previous history, such as vascular factors creating blood pressure or blood supply issues, respiratory disease or Raynaud’s disease leading to episodes of insufficient oxygen, in turn leading to other conditions like obstructive sleep disorder. Previous glaucoma episodes from burnt-out pigment dispersion syndrome, steroid use, previous retinal surgery or other stuff, like raised IOPs due to excess water drinking, prolonged wind instrument playing (think tuba player) or exercise (think yoga poses or weight-lifting), may also be the culprit. With any such episodes, it may be months before changes in optic nerve cupping become apparent. Since approximately two thirds of NTG does not progress, nothing can be taken on face value and a good search beneath the surface can be illuminating and possibly delay or prevent unnecessary treatments, he said. The three golden questions, he added, are is it glaucoma? Is it getting worse? And, if it is, how quickly?
Dr Corbett also reminded us that the trial of accommodating IOLs will soon be concluded, while Dr Alison Pereira brought the evening to a close by announcing a new research study for people who have experienced sudden vision loss due to retinal vein occlusion (RVO).
Known as the TOPAZ study, its purpose is to evaluate a new drug for reducing inflammation and the combined use of two drugs that help reduce excess fluid in the eye. Apart from participating in some valuable research, patients will benefit from very close monitoring of their eye and general health for the duration of the trial. For more information email research@aucklandeye.co.nz
We look forward to hearing more next year at Insight 2019!