Low dose atropine and ortho-k: is it OK?
The literature has established that both orthokeratology (ortho-k) and atropine are effective at slowing myopia progression and are increasingly being used clinically, including here in New Zealand. This has led to many clinicians and researchers asking the question, would combining ortho-k and atropine cause a greater reduction in myopia progression?
The exact mechanism of action for these therapies are yet to be confirmed. The working theory, however, is atropine blocks the muscarinic receptors in the retina and sclera to mediate elongation of the globe, whilst ortho-k appears to act on the peripheral retinal defocus. Thus, there could be a potential synergistic effect of combining the two therapies, with some early clinical studies shedding some light on this interesting question.
A retrospective review by Wan et al titled, The Synergistic Effects of Orthokeratology and Atropine in Slowing the Progression of Myopia, was published in the Journal of Clinical Medicine in 2018. The study examined a total of 179 files of patients with myopia who had been prescribed myopia management, either ortho-k monotherapy (n=95) or dual therapy of ortho-k and low dose atropine (n=84). The analysis further divided the groups by spherical refraction into low and high myopia with a cut-off point of over 6D considered high myopia. Those receiving atropine treatment were split again based on the concentration of atropine used, 0.025% or 0.125%. The result of this categorisation is small numbers in each group reducing the statistical quality of these results.
However, regardless of the concentration of atropine used or myopia severity, combination therapy had significantly less axial elongation and less myopic refraction progression than case-matched ortho-k monotherapy patients. This appears to suggest that the combination of ortho-k and low dose atropine may provide improved control of myopia progression than ortho-k alone. This study is, however, retrospective and patients were not randomly assigned to a treatment potentially biasing patient selection. Also, the atropine doses used do not correlate to the 0.01% that is traditionally used in New Zealand, although higher dosages of 0.02% and 0.05% are starting to be used here now too.
A second study from 2018 was a prospective, randomised control trial by Kinoshita et al, which looked at the additive effects of ortho-k and atropine 0.01% in slowing axial elongation in myopic children after one year. The prospective and randomised nature of this study, although small, provides stronger evidence of the impact of the combination therapy of ortho-k and low dose atropine compared to ortho-k alone.
A total of 40 Japanese children, aged 8-12 years old with spherical equivalent refraction between 1 and 6DS participated. Participants were split evenly between ortho-k monotherapy and dual therapy with ortho-k and atropine 0.01%. Baseline measurements for the primary outcome of axial length were taken after three months of successful ortho-k wear. One year after baseline measurements, there was statistically significantly less axial elongation in the combination treatment group of 0.09±0.12mm compared to the ortho-k monotherapy group, 0.19±0.15mm (P = 0.0356). The randomisation procedure controlled for age and spherical equivalent refraction, and no difference in age, gender, spherical equivalent refraction, axial length or visual acuity were present at entry into the study. This difference is important, with the combination being 53% more effective than monotherapy, indicating potential for combining both therapies.
These interesting papers indicate some promise in the area of dual ortho-k and low dose atropine therapy but more research is required to provide sufficient evidence of the benefits and potential risks of combining treatments. However, this research is just around the corner with a large prospective, randomised trial, the Atropine with Orthokeratology (AOK) study, with a two-year follow up, due to have results in 2020. The methods and initial results have been published as Combined Atropine with Orthokeratology for Myopia Control: Study Design and Preliminary Results in Current Eye Research this year.
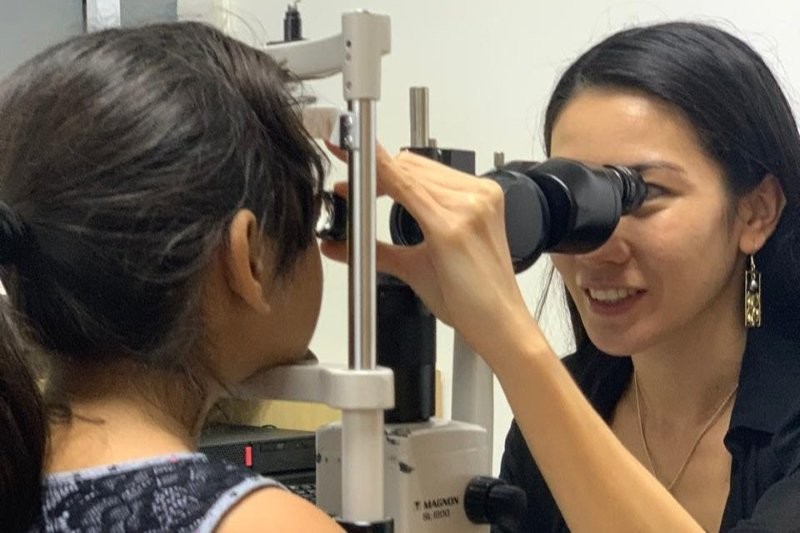
A stepwise clinical approach is often recommended to determine the efficacy of each treatment in a given individual with discussions of the risk and benefits of each treatment in turn. Anecdotally, one of our authors has used this combination therapy for several high-risk patients (long axial length at a young age, with axial progression with monotherapy) who tolerated it well. Often the atropine drop is used at dinner time or in the morning on waking, rather than before bed as usual, so as not to interfere with the ortho-k lens insertion process.
As evidence-based practitioners, we should be discussing the available evidence with our patients. For combined ortho-k and low dose atropine, the evidence is currently limited but appears positive. But is this impact limited to a subset of children with myopia? Does age, outside time, near work, severity of myopia or starting axial length change the outcomes? Only time and research will tell - watch this NZMAG space!
References:
- Wan L, Wei CC, Chen C, et al. The Synergistic Effects of Orthokeratology and Atropine in Slowing the Progression of Myopia. Journal of Clinical Medicine. 2018;7(9):259.
- Kinoshita N, Konno Y, Hamada N, et al. Additive effects of orthokeratology and atropine 0.01% ophthalmic solution in slowing axial elongation in children with myopia: first year results. Japanese journal of ophthalmology. 2018 Sep 1;62(5):544-53.
- Tan Q, Ng A, Cheng G, Woo V, Cho P. Combined Atropine with Orthokeratology for Myopia Control: Study Design and Preliminary Results. Current Eye Research. 2019 (just accepted).
This is the first edition of the new quarterly column brought to you by the NZ Myopia Action Group (NZMAG). The NZMAG is a recently-formed multidisciplinary group including optometrists, ophthalmologists, general practitioners and paediatricians, all of whom are committed to improving myopia management for children in New Zealand. This column will present up-to-date and interesting research on myopia and its management. Each column aims to present the data and current evidence on a particular area of this vast and rapidly progressing field. We hope this column will help you translate these research developments from the laboratory and the literature to becoming a part of your everyday, evidence-based practice.