MIGS, life-threatening diagnoses and trials
Auckland Eye’s North Shore Insight seminar got off to great start with attendees being asked to set up their phones so they could take part in a live quiz after the three-part seminar.
MIGS
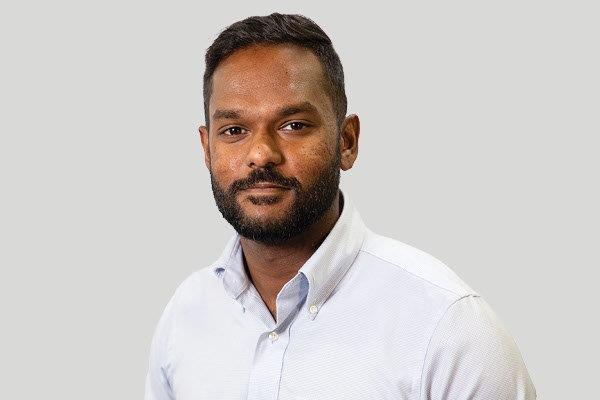
First up was Auckland Eye’s minimally invasive glaucoma surgery (MIGS) expert, Dr Shenton Chew. Dr Chew profiled three different types of MIGS devices - the iStent, Xen gel stent and MicroPulse laser (not strictly a MIGS device) - and discussed cases where each would be suitable. MIGS was preferable to traditional surgery, which was typically more labour intensive with higher risks. It may do away with the need for decades of eye drops and is useful for controlling early to moderate disease, while leaving the way open to consider a trabeculectomy or shunt in the future. It also suited cataract patients whose disease was stable, and those with progressing or advanced disease where the alternative treatment risks were too high, he said.
Diagnoses not to miss
Paediatric ophthalmologist, Dr Yvonne Ng discussed, Diagnoses you do not want to miss, sharing unusual cases she’d seen and touching on challenges examining children. The unusual findings she’s come across include Hollenhorst plaques (associated with severe cardiovascular and cerebral disease and increased mortality); amaurosis fugax (transient, sudden monocular loss of vision), often described by patients as “a curtain coming down or up”; and asymptomatic retinal emboli, an important marker for carotid disease. She also stressed the need to follow up and repeat a full exam if the patient was uncooperative, citing instances where an initial diagnosis of accommodative esotropia turned out to be medulloblastoma; what appeared to be Horner’s syndrome was, in fact, carotid artery dissection; and where slight changes in optic nerve colour and a vertical step in visual field analysis were the only signs of compressive optic neuropathy.
Dr Ng stressed the importance of being aware of other neurological developmental abnormalities, remembering acute onset comitant strabismus may be a result of vision loss from retinoblastoma or posterior fossa tumor, checking for relative afferent pupillary defect (RAPD) and trying to complete a fundus exam despite patient resistance. Dr Ng suggested distraction was often an effective way of getting children to cooperate, while wrapping infants in a blanket with their arms tucked firmly by their sides is also helpful. With regard to anterior visual pathway tumours, Dr Ng also urged caution, showing how macular changes can distract a clinician; the importance of visual field testing and checking RAPD, colour vision and brightness perception; and taking particular care with normal tension glaucoma suspects as compressive optic neuropathy can cause optic nerve cupping and arcuate defects as well as nerve fibre bundle loss.
Trials and tests
Dr Dean Corbett concluded the evening with an overview of the near two dozen clinical trials Auckland Eye’s been involved with over the past two decades and highlighting the current trials it is involved in, including one on the fluid vision IOL. He presented a case study of a 70-year-old woman with deteriorating vision who wanted to minimise her dependency on glasses, but previous radial keratotomy, laser vision correction and developing cataracts presented biometric difficulties. The placement of an Xtrafocus pinhole sulcus IOL, usually reserved for correcting irregular corneal astigmatism, provided a great solution for her, he said.
The evening ended with Dr Corbett conducting a knowledge quiz. It was a fun way to end the evening especially when, amid much hilarity, the first question turned out to be, “How many volcanic cones are there in Auckland?” The answer was “41 - 50”. Attendees were quick off the mark in answering the remaining, more optometry-centric, multiple-choice questions, but it was Haydon Optometrists’ Amanda Snedden's speed and accuracy which earned her the top spot.