Myopia in practice – Alex Petty
Reading about best practice in myopia management is one thing but hearing about how it works in practice is quite another. In the first in a series of articles, the New Zealand Myopia Action Group asked one of its founding members, Alex Petty from Bay Eye Care, to share his experiences of myopia management and why he embarked on it in the first place.
I was always interested in contact lenses and their applications, so when I learnt that orthokeratology (ortho-k) could slow the progression of myopia in children, I was fascinated. So, I’ve offered myopia control treatments to my patients throughout my career, from setting up an ortho-k programme at Visique Naylor Palmer in Palmerston North after university (which is still going strong) to today, at my specialty practice in Tauranga.
What prompted you to act on myopia?
I have personally had a rocky road when it comes to myopia. I am a high myope of -7D with long 28mm axial lengths. As a teenager my myopia progressed year-on-year but there was no treatment available to slow things down and not enough education about the potential problems this could lead to.
Fast forward to the third year of my optometry studies and my first retinal detachment spontaneously occurred over the summer. Fortunately, with prompt self-diagnosis, I was able to get myself to Greenlane Eye Clinic on the Sunday morning of Auckland Anniversary weekend and had successful pneumatic retinopexy surgery on my left eye.
Over the next five years, I had two more macula-on retinal detachments, one in each eye. I have lots of retinal scarring and a significant inferior scotoma but fortunately retain excellent central vision and have no sign of significant cataract, which is rare after over 10 years I’m told. As you can imagine, from these experiences and an uncertain visual future looming, I am incredibly passionate about actively trying to limit myopia in my young patients so they don't end up like me!
What myopia control treatments do you offer?
I offer the full complement of proven myopia control strategies: ortho-k; multifocal soft lenses, including Misight and Naturalvue MF; and low-dose atropine. I will also refer patients to colleagues to have bifocal/progressive spectacles if needed.
Each individual case has to be considered separately but, generally, ortho-k is my preference. In terms of efficacy, the literature shows good axial length control, which is evident in real patients, and I get great feedback from patients and their parents about their results, especially in terms of lifestyle and excellent uncorrected vision. So, it’s very easy to recommend this 'magic' treatment to others.
Professionally fitting a successful ortho-k lens is also very rewarding - 6/6 uncorrected vision after the first night of wear is always pretty cool!
What challenges have you faced?
Most patients and their parents are very concerned about their vision becoming more blurry during the day but struggle to understand the long-term consequences of myopia. Providing really good education content in your clinic can help people comprehend we are treating a disease, not just temporarily improving sight.
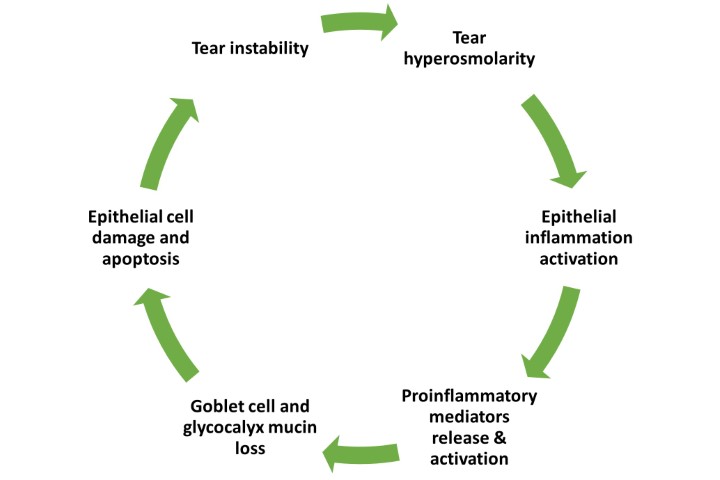
The other challenge can be trying to describe how the myopia control treatments work, especially given some mechanisms are still not completely understood. Again, good print material and resources are vital for patients to understand their options.
Have you had a particularly memorable case?
I have been fortunate in helping many myopic kids, with highly myopic parents, stop their progressive myopia in its tracks, which is incredibly gratifying for all involved! Recently, however, I had a patient with progressive myopia (-2.50DS) referred from a colleague. Corneal topography was mildly irregular and on the steep side; corneal thickness was thinner than expected; and axial length was less than expected for his refraction. The patient actually had mild central keratoconus. I’ve referred him for corneal cross-linking and he’s now doing well, corrected with single vision soft contact lenses.
Do you have any other pearls to share?
Axial length (AL) is the best metric to predict future eye health problems. Myopia ocular disease risk increases dramatically after 26mm. So, short AL patients are low risk and potentially can just be monitored, while long AL means they are high risk and need prompt myopia management.
I have seen -3.00D myopic patients younger than 10 years, some with 23mm axial lengths and others with close to 26mm! AL is also the best way to evaluate myopia progression over time, especially with ortho-k. I have an IOL master in my clinic which is ideal, however these devices are expensive, though your cataract surgeon may be happy to arrange biometry for your patients for a small fee. Some OCTs also have axial length as part of their features (eg. Optopol Revo) or, alternatively, a handheld A-scan biometer (eg. Palmscan) can work very well in a community optometry practice and costs around $2,000 to $3,000.