Neurotrophic keratitis, driving with cataracts and DED pain sensitivity
Phase II randomised, double-masked, vehicle-controlled trial of recombinant human nerve growth factor for neurotrophic keratitis
Bonini et al.Ophthalmology. 2018;125:1332-43
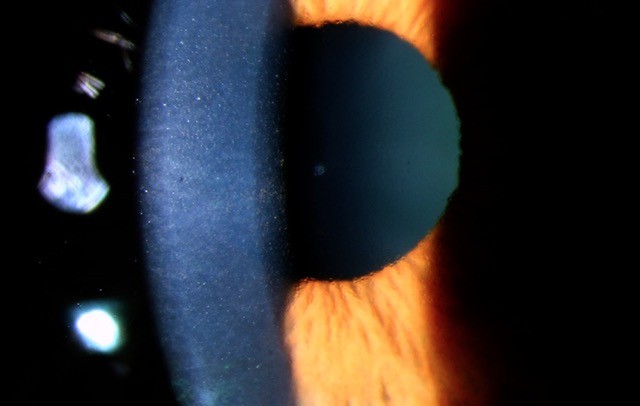
Neurotrophic keratitis (NK) is a rare corneal disease resulting from the disruption of trigeminal corneal innervation. The impairment of sensory innervation to the cornea results in a reduction of trophic neuromodulators and protective ocular reflexes essential for the vitality of the ocular surface and leads to epithelial desiccation and eventual ulceration. A wide range of ocular and systemic conditions, including herpetic keratitis, ocular chemical burns, corneal surgery, diabetes, multiple sclerosis and neurosurgical procedures, can cause NK by damaging trigeminal innervation. Diagnosis of NK requires a high level of suspicion, complete ocular surface examination and objective measurement of corneal sensitivity. The clinical stages of NK range from corneal epitheliopathy (stage 1) to persistent epithelial defect formation (stage 2) and ulceration (stage 3), which may progress to corneal perforation.
Conventional management of NK aimed to stop the progression of corneal damage and promote epithelial healing through intensive ocular surface lubrication, antibiotic prophylaxis and possible surgical intervention in the form of tarsorrhaphy. In recent years, attempts have been made to treat the underlying cause of the disease by increasing corneal sensitivity, through topical administration of nerve growth factor or corneal neurotisation.
In this phase II trial (REPARO), patients with stage 2 or 3 NK with decreased corneal sensitivity (<40 mm as measured by the Cochet-Bonnet aesthesiometer) and no objective evidence of improvement in the corneal lesion during the prior two weeks were recruited from 32 centres in six European countries.
One hundred and fifty-six patients were treated with cenegermin, a topical formulation of human nerve growth factor (rhNGF) produced in E. coli bacteria. Patients were randomly assigned 1:1:1 to treatment with cenegermin 20 mcg/mL, cenegermin 10 mcg/ mL, or vehicle, six times daily for eight weeks. All patients were followed for 48 weeks after completing treatment. The primary endpoint was percentage of eyes achieving corneal healing at four weeks.
The study results showed a highly statistically significant difference favouring both concentrations of cenegermin over vehicle (54.9% and 58.0% versus 19.6% p < 0.001 for both comparisons). The response was dose dependent with 96% of patients who responded to cenegermin remained healed at 48 weeks. Overall, the results from those assessments favoured cenegermin versus vehicle, although the differences between groups were not always statistically significant at all time points, likely due to insufficient sample size.
There were no clinically significant ocular or systemic adverse events during the treatment or follow-up periods, with ocular discomfort and abnormal eye sensation being the most common reported adverse effects. A parallel study has led to FDA approval of cenegermin (Oxervate) in the United States. Corneal specialists eagerly await the commercial availability of this drug to help with the medical management of recalcitrant neurotrophic keratitis.
Association of cataract surgery with traffic crashes
Schlenker et al. JAMA Ophthalmology, 2018; 1;136(9):998-1007
Worldwide, traffic crashes account for over one million deaths annually, with drivers older than 65 years representing the highest level of risk. Cataracts have previously been thought to increase a driver’s risk of a serious traffic accidents as they decrease driving performance.
In this population-based longitudinal study carried out in Ontario, Canada, more than 500,000 consecutive patients over 65 years of age undergoing cataract surgery were evaluated over a 10-year period. The mean age of the population was 75 years and each patient was observed for four years before surgery and at least one year after surgery for accidents whilst driving a car, motorcycle or bicycle.
A total of 4680 traffic crashes (2.36 per 1000 patient-years) accrued during the 3.5-year baseline interval and 1200 traffic crashes (2.14 per 1000 patient-years) during the one-year subsequent interval, representing 0.22 fewer crashes per 1000 patient-years following cataract surgery (odds ratio [OR], 0.91; P=.004). No significant reduction was observed in other outcomes, such as traffic crashes where the patient was a passenger or pedestrian, nor in other unrelated serious medical emergencies.
Overall there was a 9% reduced risk of a serious crash after cataract surgery compared to before surgery. This is a significant increase in safety and equals the benefits of an airbag being deployed in the car. It is worth highlighting that the crash rate after surgery was higher in the first postoperative month, perhaps due to overconfidence, neuro-adaption, uncorrected refractive error as well as anisometropia. This should serve as a reminder for all health care professionals to stress the importance of care to patients who start driving in the early postoperative period.
This modest reduction in risk has potential implications for mortality, morbidity and socio-economic cost to society and adds to the myriad of benefits of cataract surgery such as improved quality of life, improved odds of living longer as well as a reduced the risk of falls and hip fractures.
Pain sensitivity associated with the length of the maximum interblink period
Li et al. Invest Ophthalmol Vis Sci. 2018; 1;59(1):245-252
Dry eye disease (DED) is a chronic, multifactorial condition, with a prevalence ranging from 5-34% in the general population. It is a leading cause of patient visits to health care practitioners with an annual cost of treatment estimated to be around US$1000 in the USA. Evidence-based diagnosis and treatment is often challenging in this condition which can significantly impact a patient’s quality of life. Whilst a large body of research has been completed on the field, one enduring question yet to be solved is why discrepancies exist between clinical signs and patient reported symptoms in DED.
In this study the authors hypothesised that this discrepancy was linked with the diverse levels of subjective pain perception, where the same injury can be reported as mild irritation by some, but as severe pain by others. The investigators recruited 42 healthy subjects (36 females), with a mean age of 23 years. Participants were asked to complete the Pain Sensitivity Questionnaire, and subsequently underwent evaluation to assess interpalpebral area, tear meniscus height, ocular surface cooling, tear-film lipid layer thickness and non-invasive tear break-up time. It is worth noting that the primary painful stimuli in DED are thought to be greater ocular surface cooling and tear hyperosmolarity as a result of increased tear evaporation and the investigators measured ocular surface cooling rate on the eye using a thermographer with a 0.1°C thermal sensitivity.
Subjects were then asked to refrain from blinking until they felt discomfort and this period between blinks was timed; maximum interblink period (MIBP). Researchers found that a longer MIBP was associated with decreased pain sensitivity (P = .04), lower ocular surface cooling rate (P < .001) and Asian ethnicity (P = .005).
The authors estimated that individuals would have be able to refrain from blinking for an additional four seconds if they had the lowest (0.6) compared to the highest (6.1) pain sensitivity in the cohort. The investigators postulated that baseline corneal sensitivity to pain (unaffected by contact lens wear or dry eye) is associated with an individual’s pain sensitivity. This assertion requires further investigation as greater corneal sensitivity to pain can also be a by-product of DED.
Although small, this study has shed some light on the complex nature of ocular surface pain perception and the role of ethnicity on DED symptoms. Asians have previously been reported to have greater tear-film instability and increased corneal staining compared to non-Asians which suggest that they are exposed to a higher frequency and greater magnitude of noxious stimuli on the ocular surface. It should be noted that the subjects recruited were young, healthy and predominantly female and the results can not necessarily be applied to other populations.
About the author
Dr Mo Ziaei is a cornea and anterior segment surgeon, with quadruple fellowship training from Moorfields Eye Hospital (London) and New Zealand National Eye Centre (Auckland). He works as an honorary senior lecturer at the University of Auckland and as a specialist at the Re:Vision sight correction centre.