Ocular allergy and dry eye
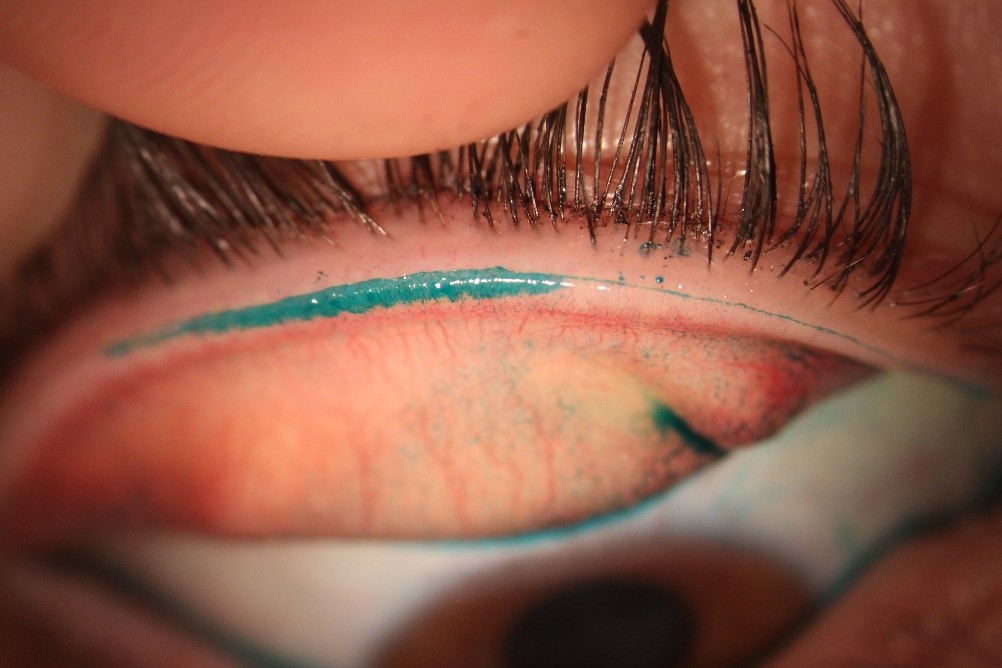
Ocular allergy represents a group of hypersensitivity disorders that primarily affects the conjunctiva.
The most common form of ocular allergy is seasonal allergic conjunctivitis (SAC), accounting for 90% of cases. The most prevalent allergens in SAC are grass, tree and weed pollen, and outdoor moulds. In the United Kingdom, the prevalence of ocular allergy to grass pollen in patients attending optometric practice is estimated to be 8% – no data is currently available from Australasian countries.
Similar to dry eye, although the signs and symptoms of SAC are usually mild, they may hinder school performance, work productivity and everyday tasks such as driving. The primary treatment strategy for SAC involves avoidance of the offending allergen to prevent the initiation of the allergic response. However, complete avoidance is not often possible and use of topical anti-allergic medications is required when signs and symptoms occur. While non-pharmacological treatments, such as artificial tears developed for dry eye and cold compresses have been used for many years, in conjunction with allergen avoidance strategies and anti-allergic medications to help bring about symptomatic relief, evidence showing the effectiveness of this approach has only relatively recently been published. In this study, patients had controlled exposure to grass pollen and either used cold compresses or artificial tears, resulting in therapeutic effects on the signs and symptoms of allergic conjunctivitis. A cold compress enhanced the use of epinastine (a mast cell stabiliser/antihistamine combination) and was the only treatment to reduce symptoms to baseline within an hour of antigenic challenge. Signs of allergic conjunctivitis were generally reduced most by a combination of cold compress and artificial tears or epinastine.
In a separate, recent study, acute allergic rhinoconjuctivitis has been shown to be characterised by tear hyperosmolarity, which can be rehabilitated with the administration of hypotonic artificial tears, much like dry eye.
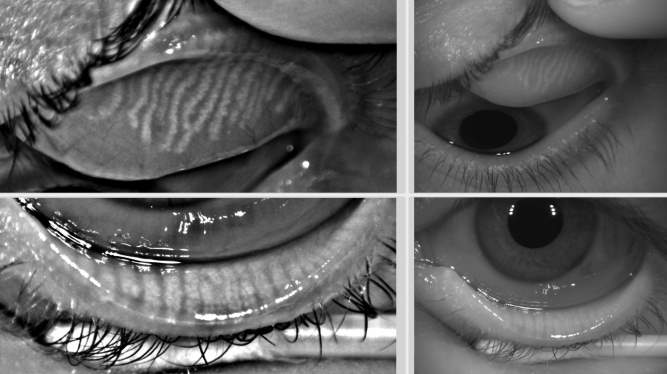
Considerable overlap of reported symptoms of itch and dryness has been reported in groups with presumed dry eye and seasonal allergic conjunctivitis. As with ocular allergy, there can be seasonal (summer and winter) and weather-related aspects to dry eye symptoms. Similar biomarkers for the biological ‘diagnosis’ of both dry eye and ocular allergy have been proposed, along with imaging techniques such as in-vivo confocal microscopy, but these have not been adopted clinically.
Dry eye symptoms are generally greater in those with ocular allergy and some ocular allergy medications can induce signs and symptoms of dry eye. Hence it would seem that clinically the conditions are often confused and careful questioning of when the symptoms occur is advised to aid with the selection of appropriate management.
References
Abelson MB, Leonardi A, Smith L. The mechanisms, diagnosis and treatment of allergy. Rev Ophthalmol 2002;9:74-84.
Bielory L. Ocular allergy overview. Immunology Allergy Clin 2008;28:1-23.
Wolffsohn JS, Naroo SA, Gupta N, Emberlin J. Prevalence and impact of ocular allergy in the population attending UK optometric practice. Contact Lens Ant Eye 2011;34:133-8.
Smith AF, Pitt AD, Rodruiguez AE, et al. The economic and quality of life impact of seasonal allergic conjunctivitis in Spanish setting. Ophthalmic Epidemiol 2005;12:233-42.
Bielory L. Ocular allergy treatment. Immunology Allergy Clin 2008;28:189-224.
Chigbu DI. The management of allergic eye disease in primary care. Contact Lens Ant Eye 2009;32:260-72.
Bilkhu PS, Wolffsohn JS, Naroo SA, Robertson L, Kennedy R. Effectiveness of non-pharmaceutical treatments for acute seasonal conjunctivitis. Ophthalmology 2014;121:72-8.
Nitoda E, Lavaris A, Laios K, Androudi S, Kalogeropoulos CD, Tsatsos M, Damaskos C, Garmpis N, Moschos MM. Tear Film Osmolarity in Subjects with Acute Allergic Rhinoconjunctivitis . In Vivo 2018;32:403-8.
Hom MM, Nguyen AL, Bielory L. Allergic conjunctivitis and dry eye syndrome. Annals Allergy, Asthma, Immunol 2012;108:163-6.
van Setten G, Labetoulle M, Baudouin C, Rolando M. Evidence of seasonality and effects of psychrometry in dry eye disease. Acta Ophthalmol 2016;94:499-506.
Enriquez-de-Salamanca A, Bonini S, Calonge M. Molecular and cellular biomarkers in dry eye disease and ocular allergy. Curr Opin Allergy Clin Immunol 2012;12:523-33.
Villani E, Mantelli F, Nucci P. In-vivo confocal microscopy of the ocular surface: ocular allergy and dry eye . Curr Opin Allergy Clin Immunol 2013;13:569-76.
Vehof J Smitt-Kamminga NS, Nibourg SA, Hammond CJ. Predictors of discordance between symptoms and signs in dry eye disease. Ophthalmol 2017;124:280-6
Ousler GW, Workman DA, Torkildsen GL. An open-label, investigator-masked, crossover study of the ocular drying effects of two antihistamines, topical epinastine and systemic loratadine, in adult volunteers with seasonal allergic conjunctivitis. Clin Therapeutics 2007;29:611-6.
Professor James Wolffsohn is pro-vice chancellor of Aston University, Birmingham, England and was a sub-committee chair for TFOS DEWS II. His main research areas include the development and evaluation of ophthalmic instrumentation, contact lenses, intraocular lenses and the tear film.