OTC 2019: Debates and side effects
Side effects and debates was the promise of this year’s Ocular Therapeutics Conference and it most certainly delivered.
The conference’s scientific committee selected topics and questions we as clinicians wrestle with regularly. This year, this included two key areas: myopia management and the ocular effects of systemic medication, both of which were covered wonderfully at the conference.
The great myopia debates
The myopia controversies round started with a bang! Imagine Rocky music playing, people cheering, speakers running down the aisle and quick-witted banter. The discussions we often have with colleagues, or sometimes just with ourselves, were presented and played out in front of us. First up, Dr Rasha Al-Taie, a paediatric ophthalmologist, and Dr John Phillips, an optometrist and leading researcher in myopia control from the University of Auckland’s School of Optometry and Vision Science, debated the use and efficacy of low dose atropine (0.01%).
Some recent, shorter-term data has shown there is little to no impact on axial length elongation with this treatment despite a surprising decrease in the rate of refractive change. However, the ATOM (atropine for the treatment of myopia) 1 and 2 studies both showed a reduction in axial length elongation with higher dose atropine treatments. It was argued therefore, that the dosage of atropine used for myopia control could just be increased. However, with increased concentration side effects, such as dilated pupils, reduced accommodation and the potential for adverse events or allergic responses, must be considered.
In the discussion time following this lively debate the best approach was considered to be starting children on the lowest dose and, if axial elongation persists, slowly increasing the dose whilst monitoring for side effects or adverse events. This approach may prevent over-treating as the data appears to show control of myopia progression with 0.01% in some children, though longer and more detailed research is required in this exciting and rapidly expanding field.
Atropine is not our only option for myopia control, however, and Rasha and John’s discussion led nicely to the next big debate of the day, To ortho-k or to not ortho-k, presented by Alex Petty, an optometrist and orthokeratology specialist, and Dr Akilesh Gokul, a contact lens specialist optometrist and research fellow at the University of Auckland, who came ready for battle complete with boxing gloves.
Alex highlighted that ortho-k has been proven to reduce the axial length elongation of the eye, children and their families enjoy glasses-free vision and the rate of associated keratitis has significantly decreased. In contrast, Aki pointed out that although there have been many improvements in ortho-k, it still poses a higher risk of infection compared to daily contact lens wear, corneal nerves remodel overtime with ortho-k wear and the range of powers correctable by ortho-k is still limited.
So, we still ask, to ortho-k or not to ortho-k, to atropine or not? The big questions are still there; there are no clear-cut answers but what we do know is that we have to do something about the myopia epidemic. There is evidence for atropine and for ortho-k. Maybe ortho-k reduces the axial length more, but atropine can be more effective at reduction in refraction. What was made clear by all speakers is that as eye care professionals, we need to do something. We have to talk to patients about their options and about the evidence we currently have. We have to encourage our patients and our patients’ parents that spending time outside, away from screens is a great way to ward off myopia. We have to stay informed in this rapidly changing field. All speakers also recommended measuring axial length as a core test to accurately monitor, manage and, if needed, act to control myopia.
Ocular side effects of systemic meds
Professor Charles McGhee opened this core session with an overview of common ocular side effects, including corneal deposits, intra-ocular pressure changes, changes in pupil size and reactivity, retinal changes, optic neuritis and diplopia. The wide variety of side effect presentations mean, that as clinicians, we need to ensure we are aware of all medications patients are taking. Prof McGhee also reminded us that patients often fail to mention over-the-counter medications or health supplements and it’s helpful to ask about different medicines and supplements administration routes, for example, whether they are infusions, inhalers, ointments or oral medications.
During the remainder of the session, the audience was reminded of common ocular side effects from common medications by several interesting speakers, including Drs James McKelvie, Monika Pradhan and Taras Papchenko. These included:
- Digoxin, commonly used for the treatment of atrial fibrillation or atrial flutter - can have toxic effects on the retina and can impair colour vision
- Zolendronate, an infusion used for osteoporosis - causes acute anterior uveitis in 1% of cases within one week of receiving the dose
- Tamoxifen, an oral antiestrogen medication used in the prevention and treatment of HER2+ breast cancer - can cause crystalline ‘glittery’ deposits on the corneal endothelium which can be reversed with cessation of the medication. However, retinal crystalline deposits can also form that don’t appear to resolve on cessation of use
- Hypnotics, such as benzodiazepines which are commonly used to help with sleep, relax muscles and to treat anxiety, epilepsy and alcohol withdrawal. These affect the central nervous system and can cause changes such as mydriasis and a reduction in accommodation
- Sildanafil, vardenafil or tadalafil, more commonly known as Viagra, or similar products can result in colour vision changes with a blue or violet tint as well as blurred vision
- Hydroxychloroquine – an immuno-modulator used in the treatment of rheumatoid arthritis and lupus, can result in bulls eye maculopathy and reduced vision. The affect is cumulative dose-related and therefore there are clear screening guidelines which can be found through the American Academy of Ophthalmology.
However, this list barely scratches the surface of ocular impacts of systemic drugs. Sometimes medication side effects can seem overwhelming. The key clinical pearl I took home, however, is that we probably won’t know all of them, but what we can do is take an extremely thorough history and then look up what we do not know. There are excellent resources available including the New Zealand Universal List of Medicines and Medsafe data sheets (www.medsafe.govt.nz) which should be used regularly by all eye care practitioners.
In conclusion
The annual Ocular Therapeutics Conference is always a high point in the events calendar with great topics tackled, up-to-date therapeutic knowledge and amusing but ultimately informing debates. A huge thank you to the Buchanan Ocular Therapeutics Unit and the sponsors for making the event possible.
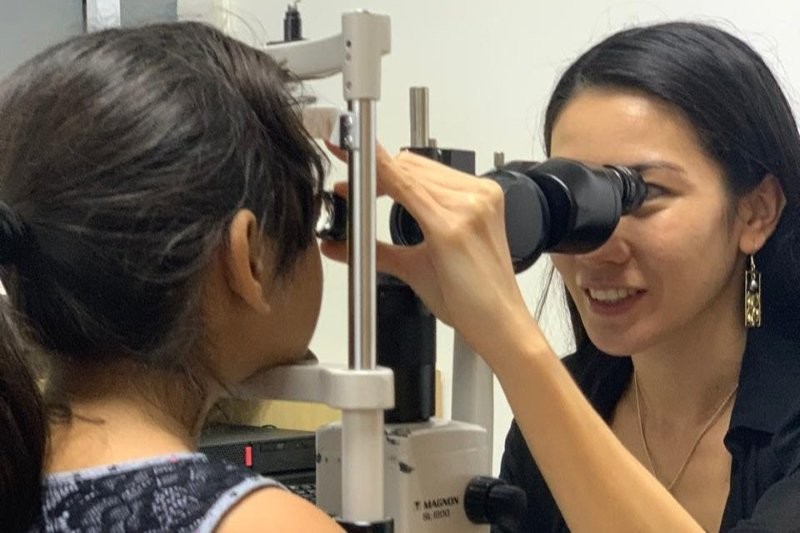
Dr Samantha Simkin is a therapeutically-qualified optometrist, a member of the BLENNZ National Assessment Team and the Stevenson post-doctoral research fellow at the University of Auckland.