Research reviews: retinal detachment with macula-off, epiretinal membranes and anti-VEGF for DMO
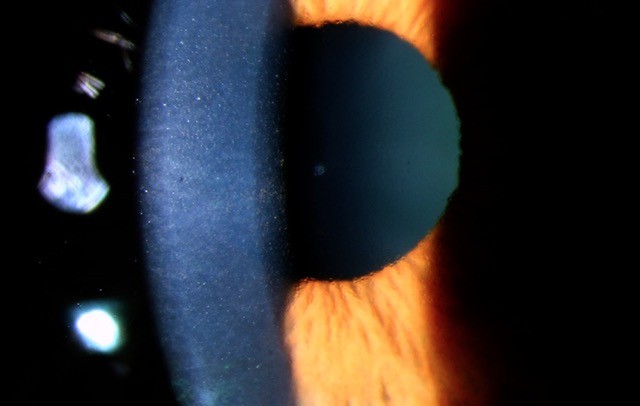
Visual recovery after retinal detachment with macula-off: is surgery in the first 72h better?
Frings A, Markau N, Katz T et al
British Journal of Ophthalmology. 2016;100:1466 -1469
Unlike macula-on retinal detachment, which is often treated as an “ophthalmic emergency” and repaired swiftly before the macula detaches, macula-off retinal detachment is usually considered less of an emergency. However, determining the ideal time for repair of macula-off retinal detachment before compromising the visual prognosis can be difficult. The purpose of this study was to evaluate the influence of lag-time between the onset of central visual acuity loss and surgical intervention of macula-off retinal detachment.
A retrospective review of 1727 patients was undertaken, with 89 patients meeting the inclusion criteria. The main outcome measure was final visual acuity as a function of symptom duration of macula-off detachment. Symptom duration was defined as the time from the onset of loss of central vision (macula detachment) to surgical intervention.
The results showed there was no clinically significant difference in final visual acuity in those operated within 10 to 30 days of macula-off retinal detachment. But patients with symptom duration of three days or less achieved best final visual acuity (p<0.001).
Comment:
This study suggests we should aim to repair macula-off retinal detachments within three days of the macula detaching. After 10 days of central visual acuity loss, the final visual outcome is clinically comparable and independent of further delay of surgery up to 30 days. Therefore, in some cases, surgery for macula-off retinal detachment may be postponed without compromising the patient’s visual prognosis.
Prognostic factors of epiretinal membranes: A systematic review
Miguel A, Legris A.
Journal Français D'Ophtalmologie. 2017 Jan;40(1):61-79
Deciding when to refer patients with epiretinal membrane, who will do well with epiretinal membrane surgery, can be difficult. The purpose of this systematic review was to review the prognostic factors of epiretinal membrane after surgery.
Inclusion criteria were: 1) primary purpose was to identify a prognostic factor epiretinal membrane; 2) prospective or retrospective study, case series (more than 10 patients), or clinical trials; 3) follow-up of at least three months; 4) complete ophthalmological evaluation in each patient with visual acuity and OCT, preoperative and ≥3months after surgery; 5) vitrectomy with epiretinal membrane peeling performed in each patient.
A total of 21 studies were included (nine prospective, 12 retrospective). Prognostic factors for visual acuity (VA) improvement after epiretinal membrane surgery included: shorter duration of symptoms before surgery, reduced central foveal thickness at baseline identified by optical coherence tomography (OCT), good integrity of the inter segment/outer segment photoreceptor junction at baseline, and thinner ganglion cell inner plexiform layer at baseline.
Comment:
This study implies that patients with epiretinal membrane should perhaps be referred for consideration of epiretinal membrane surgery earlier than traditionally recommended, before foveal thickness becomes too great and retinal integrity is compromised.
Anti-VEGF for diabetic macular oedema: a network meta-analysis
Virgili G, Parravano M, Evans JR et al
Cochrane Database of Systematic Reviews. 2017 Jun 22;6:CD007419.
Previous studies have found anti-vascular endothelial growth factor (anti-VEGF) therapy to be effective in treating diabetic macular oedema. However, with multiple anti-VEGF therapies available, including aflibercept (Eyelea), bevacizumab (Avastin) and ranibizumab (Lucentis), it can be difficult to decide which is the best treatment option.
The aim of this Cochrane Review was to determine the best type of anti-VEGF medication for the treatment of diabetic macular oedema (DMO).
A total of 24 relevant studies were identified. The review found that all three anti-VEGF medications prevented visual loss and improved vision in people with DMO, however those receiving ranibizumab were less likely to improve vision compared with aflibercept.
Approximately three in 10 people improved vision by three or more lines with ranibizumab and one in 10 additional people achieved this with aflibercept. People receiving ranibizumab and bevacizumab have a similar visual outcome at one year after the start of treatment. The risk profile for all three medications was similar.
Comment:
All three anti-VEGF options can help to improve vision in people with diabetic macula oedema. However, aflibercept probably offers some advantage over ranibizumab and bevacizumab. It should be noted that evidence from such studies may not always translate to clinical practice, perhaps even more so in New Zealand where the availability of aflibercept is limited and its cost much greater than bevacizumab. Bevacizumab costs less than $100 per injection compared to $1,250 for ranibizumab or $1,650 for aflibercept (PHARMAC 2016).
About the author:
*Dr Will Cunningham, a cataract, medical retina and vitreoretinal surgeon, splits his time between Auckland District Health Board and Eye Institute. He returned to New Zealand in 2017 after completing two fellowships in vitreoretinal surgery, and is expanding his expertise in ocular oncology.