Retinal detachment, vitreopathy and photocoagulation treatment reviews
Choice of primary rhegmatogenous retinal detachment repair method in US commercially insured and Medicare Advantage patients, 2003-2016, Reeves M, Pershing S, Afshar A
American Journal of Ophthalmology, Volume 196, p.82-90
Review
With the evolution of modern vitrectomy surgery, more traditional methods such as scleral buckling and pneumatic retinopexy for the repair of primary retinal detachment are becoming less common, with some surgeons choosing to avoid using these techniques altogether.
The purpose of this study was to evaluate trends in retinal detachment repair between 2003 and 2016. They identified 31,995 retinal detachments over the study period. As expected, pars plana vitrectomy (PPV) was consistently the most common repair technique, increasing over time, with scleral buckling declining. PPV was more likely in patients with pseudophakia and vitreous haemorrhage. Lattice degeneration and younger age were associated with higher odds of scleral buckling. Pneumatic retinopexy was more likely among patients with better systemic health and less likely in those with vitreous haemorrhage or lattice degeneration.
Comment
This study confirms that PPV is the most common technique for primary RRD repair in the US and New Zealand statistics would likely reflect this too. However, more traditional techniques such as scleral buckling and pneumatic retinopexy still have their place in the repair of primary retinal detachment. In selected cases it can produce excellent rates of reattachment with the potential for fewer complications such as cataract.
Personally, I perform on average two scleral buckling procedures per month and find them very useful, particularly in younger patients without a posterior vitreous detachment and in cases with advanced proliferative vitreoretinopathy (PVR) or subretinal bands.
Long-term safety and efficacy of limited vitrectomy for vision-degrading vitreopathy resulting from vitreous floaters, Sebag J, Yee K, Nguyen J et al.
Ophthalmology Retina, September 2018, p.881–887
Review
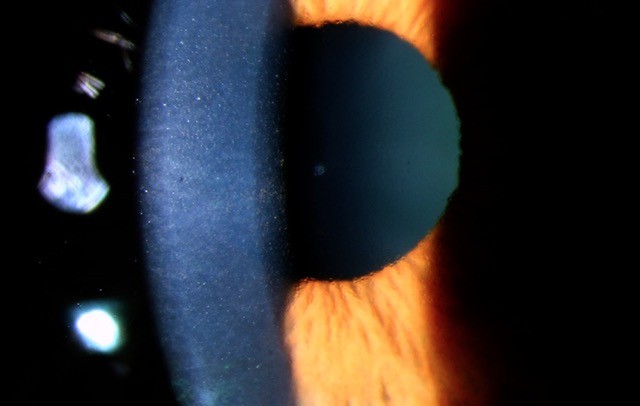
Most vitreous floaters (not related to any sinister ocular pathology) become less symptomatic over time. However, in some patients, vitreous floaters can have a significant impact on vision and quality of life to the extent that surgical removal is warranted.
This study analysed 145 patients who underwent “limited” 25g vitrectomy (vitrectomy without the removal of anterior vitreous adjacent to lens and without induction of posterior vitreous detachment) for bothersome floaters. Follow-up averaged 33 months and outcome measures included visual acuity, a 39-item National Eye Institute Visual Function Questionnaire (VFQ) results, contrast sensitivity function (CSF – Weber Index) and quantitative ultrasonography results.
Researchers found that after surgery vitreous echodensity decreased by 94.1% (P < 0.0001) and VFQ results improved by 19.3% (P < 0.0001). Preoperative VA was 0.68 ± 0.21, improving to 0.77 ± 0.19 after surgery (P < 0.0001). Preoperative CSF was degraded by 91.3% compared with controls (P < 0.0001), normalising at 1, 3, 6, 12, 24, 36, and 48 months after surgery (P < 0.00005 for each). There were no cases of endophthalmitis. There were three retinal tears and three retinal detachments that underwent successful repair. Cataract surgery occurred in 21 of 124 patients (16.9%; mean age, 64 ± 7 years; none younger than 53 years), at an average of 13.1 ± 6.8 months after vitrectomy.
Comment
This study confirms that removing symptomatic vitreous floaters can significantly improve vision and quality of life. However, it was surprising that the study reported three retinal detachments, as this rate is much higher than audited results suggest across Australasia. One possible explanation for a higher complication rate in this study was performing a “limited” vitrectomy without PVD induction, allowing residual vitreous to place traction on the retina inducing a retinal tear or detachment postoperatively.
I’m sure most of my vitreoretinal colleagues would agree that with modern small gauge vitrectomy techniques, we can quite safely perform a “complete” vitrectomy for patients with bothersome floaters (or any other vitreoretinal condition) with much improved complication rates than suggested in this study.
Five-year outcomes of pan-retinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomised clinical trial, Gross J, Glassman A, Liu D et al; Diabetic Retinopathy Clinical Research Network
JAMA Ophthalmology, 2018 Jul 24
Review
We have traditionally treated proliferative diabetic retinopathy (PDR) with pan-retinal photocoagulation (PRP). However, with the advent of intravitreal anti-VEGF agents such as bevacizumab (Avastin) and ranibizumab (Lucentis), we now have many more options to choose from when treating this potentially blinding and sometimes very aggressive disease.
In this study, one of the leading research groups in diabetic retinopathy (DRCR.net) set out to evaluate the efficacy and safety of 0.5-mg intravitreous ranibizumab vs pan-retinal photocoagulation (PRP) for the treatment of PDR.
This large multicentre randomised clinical trial evaluated 394 eyes and found that severe vision loss or serious PDR complications were uncommon with PRP or ranibizumab. However, the ranibizumab group had lower rates of vision-impairing diabetic macular oedema with a cumulative probability of 22% compared with 38% in the PRP group. There was also less visual field loss in the injection group, with a mean (SD) change in cumulative visual field total point score of -330 dB vs -527 dB in the PRP group.
Comment
These findings support the use of intravitreal anti-VEGF agents in the treatment of PDR. However, one must consider other factors influencing our treatment of choice aside from a reduced risk of field loss and macular oedema. Treatment compliance (often poor amongst diabetics), frequency of visits (multiple injections vs. 1-2 sessions of laser treatment) and the cost of the treatment must all be considered, especially in our current climate where intravitreal injections for other conditions are already placing significant burden on our health system.
Dr Will Cunningham, a cataract, medical retina and vitreoretinal surgeon, splits his time between Auckland District Health Board and Eye Institute. He returned to New Zealand in 2017 after completing two fellowships in vitreoretinal surgery, and is expanding his expertise in ocular oncology.