Sharing the load, safely
One of the world’s most prestigious eye hospitals and ophthalmology training excellence, Moorfields in London, is poised to release further data on the success of its paramedical intravitreal (IVT) injection training programme and practice.
The new data will be published shortly and then released publicly, said Adam Mapani, Moorfields’ first ophthalmology nurse consultant. “It’s been very successful. When the injections were first made available, waiting time was something like eight weeks and now with nurses’ involvement, it’s about two weeks… and the safety outcomes have been absolutely amazing… (with) a lower risk of endophthalmitis compared with doctor-led injections.”
The Moorfields’ IVT programme
Moorfields started training nurses and allied health professionals to give anti-vascular endothelial growth factor (anti-VEGF) injections in 2012 after identifying they had a serious and growing supply and demand problem.
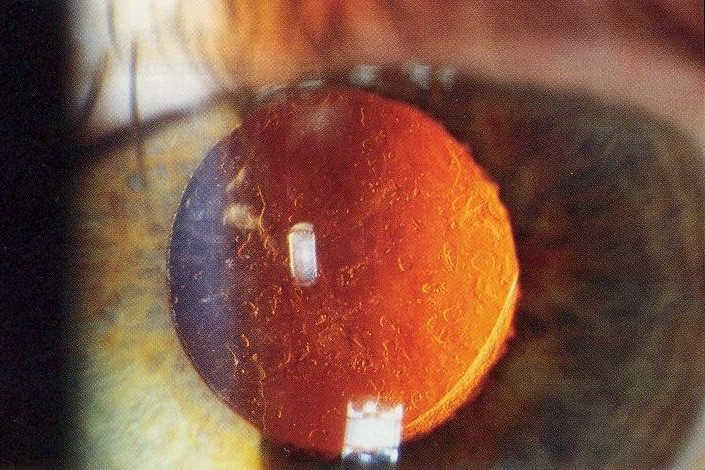
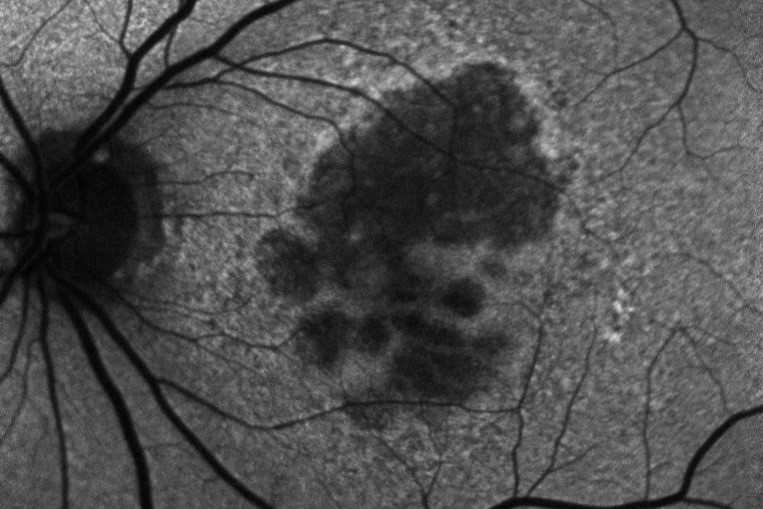
The success of anti-VEGF agents in staving off blindness from wet age-related macular degeneration (AMD) has created unprecedented demand for injections. The problem is compounded by an aging population and anti-VEGF agents being successfully indicated for other conditions, such as diabetic macular oedema and retinal vein occlusions. Thus, the decision to train other staff to give IVT injections had the full support of the Moorfields Eye Hospital NHS Foundation Trust board and the medical director at the time, said Tracy Luckett, Moorfields director of nursing and allied health professionals.
Initial data published by Mapani and colleagues in 2014 and 2015 showed the success of the programme right from the beginning. Patient safety, patient experience and clinic capacity were all measured, with no serious vision-threatening complications recorded in 4000 nurse-delivered IVT injections, no significant difference to doctor-led injections and patients providing positive feedback that they were more than satisfied with the service.
Today, more than 50 nurses provide IVT injections at Moorfields, working with consultants and allied health professional colleagues in nurse-led retina clinics. Moorfields is also sharing what it’s learnt through a one-day course designed to help others introduce a paramedical IVT injection training programme into their hospitals. Now running for five years, and three-times a year, this injection programme course is very popular, said Mapani. “We’ve trained more than 500 nurses and allied healthcare professionals inside and outside the UK, including two nurses from Melbourne and Brisbane, and one from New Zealand. It’s always full! It’s about us sharing the Moorfields journey, the medico-legal aspects, good governance and what we’ve learnt.”
Initially, actual injection training was given by senior consultants but as time has gone by, and as nurses now provide the vast majority of injections, this has also become nurse-led, said Luckett. “The future of ophthalmology is really about who is best placed to deliver the care, rather than saying, ‘a doctor needs to do this, an optometrist needs to do this and a nurse needs to do this’. There will always be some element of that because that goes with their training, competence and technical ability, but what we are trying to do and we’ve been reasonably successful doing is to say, ‘let’s forget about you being a registered doctor, nurse or optometrist, what can you be trained or developed to do’, and that’s a combination of education, competencies and skills development.”
At Moorfields, feedback on the paramedical IVT injection programme includes patients reporting they enjoy the continuity of care provided by nurses, compared with previously having to see a different doctor each time. Consultants and visiting fellows also prefer the new process, especially as visiting fellows, who used to be drafted into Moorfields’ injection clinics to help with the backlog, can now focus on more complicated cases, which is far better for their training, said Mapani. “We’ve had excellent feedback from everyone on this, especially visiting fellows.”
The Australasian perspective
Commenting on this at the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) annual conference at the end of 2019, one senior New Zealand consultant ophthalmologist, who didn’t wish to be named, agreed with Moorfields’ approach. If it wasn’t for the ophthalmic nurses in his hospital being able to give injections, he’d spend he’d spend his whole time giving anti-VEGF injections and have no time to do sight-saving surgery, he said.
Cognisant of similar workforce concerns and the rise and rise in demand for anti-VEGF injections, New Zealand began training nurses to give IVT injections in 2012. Studies published in July 2016 and November 2016 in Auckland and Wellington, respectively, showed the safety profile achieved was the same as doctors, while the move enabled far more patients to be treated in a timely fashion, saving their sight.
“In keeping with the ‘work smarter not harder’ ethos, this transfer of ‘routine’ tasks has been realised both as a cost-saving per treatment delivered, and better utilisation of medical staff time…” wrote Auckland study authors Dr Priya Samalia, David Garland and Dr David Squirrel in the July 2016 issue of The New Zealand Medical Journal. “The utilisation of suitably trained nursing staff to deliver these treatments has had a positive impact on the medical retina service, allows for better utilisation of medical staff and has improved accessibility to the service for our patients,”
In Australia last year, the latest Medicare Benefits Schedule Review Taskforce Ophthalmology Report, following advice from Australia’s Ophthalmology Clinical Committee, also recommended a review of Australia’s broader ophthalmology workforce. “In relation to this review, the taskforce recommends a specific focus to assess the expansion of intravitreal injections to include appropriately trained nurse practitioners and optometrists… in response to evidence of clinical need, maldistribution of clinicians and constraints on overall supply.”
RANZCO’s position
Talking to NZ Optics at the RANZCO conference, RANZCO board members Associate Professor Nitin Vermer and Professor Peter McCluskey, said they looked forward to reading Moorfields latest published research in this area. But RANZCO remains committed to its stance that IVT injections, should be done by medically-qualified professionals, ie. ophthalmologists, until they are convinced by the research, they said.
“A College needs to have consensus policy that everyone in the membership follows,” said Prof McCluskey. “Once this evidence is published, then RANZCO will look at it and it’s possible that in the future things might change. But at the moment, our focus is on safety and making sure there’s a consensus among RANZCO that we do things in a safe way to ensure the best patient outcomes.”
New Zealand’s problem, like Moorfields’, is a workforce issue, said Prof Vermer. “It’s a very complex issue, and if it’s something that is based on evidence, then we can start working on solutions… and what works in New Zealand might be different from what works in Australia because the systems are different… but as a College we have one position.”
When asked about where RANZCO was regarding the guidelines for nurse injectors and support for other hospital-based allied health professional involvement in this area, mooted by RANZCO CEO David Andrews in September*, Prof Vermer and A/Prof McCluskey reiterated RANZCO’s position and said there were a number of working parties discussing numerous areas.
“Yes, (we’re in discussions) absolutely, but our position remains the same,” said A/Prof Nitin. “We have a lot of things going on all the time and at this stage we don’t have any published guidelines on this. That is something we would work on if we need to… because we’re not here to hinder, we’re here to help. But we must be very sure that the help we’re giving meets international standards, meets patient safety standards, is current and so on. So, we might appear to be moving slow, but we are very cautious because we don’t want to make the wrong decision.”
In summary
“Challenges such as an aging population mean that all involved in eye care must seek to deliver services in increasingly innovative ways,” said Dr Nick Strouthidis, Moorfields medical director. “Moorfields is active in meeting this challenge in several ways, including advancing the clinical roles of our allied health professionals to have skills that are fit for the future demands of ophthalmic services.”
* www.eyeonoptics.co.nz/articles/archive/optometrists-to-give-anti-vegf/