The role of optometry in MBGS and cross-linking
The rise of webinars in our post-Covid-19 world has opened up avenues of education extending beyond borders and time zones. Hence a 7pm kick-off in Sydney saw me attend a session on discussing optometry’s role in MBGS and cross-linking, maskless and in my pajamas, with coffee and my one-eyed, three-legged cat for company, while Australian clinical optometrists Jason Holland and Phuc Ngo expounded on the finer details of the treatment of glaucoma and keratoconus.
A Google search to discover the meaning of the acronym MBGS turned up a variety of possibilities, some even relevant to ophthalmology. The clue as to what was on offer, was that this particular webinar was sponsored and hosted by Glaukos, a company known for developing the iStent inject* trabecular micro-bypass technology for minimally invasive glaucoma surgery (MIGS).
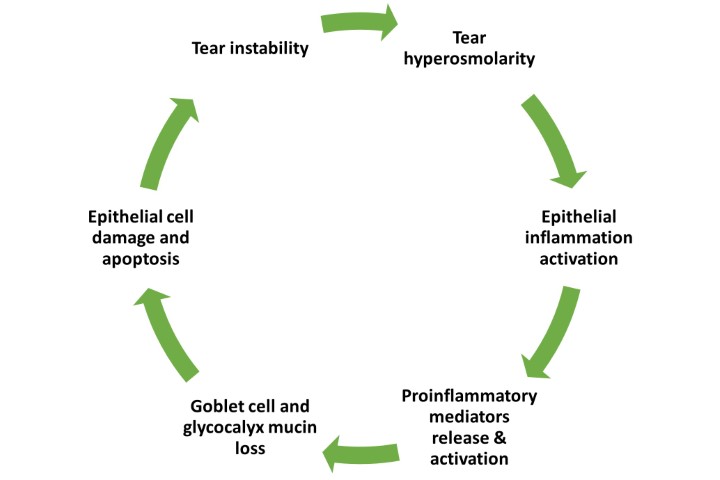
“Maintenance of the glaucoma patient,” opined Holland, “is as much of a challenge to optometrists as the initial diagnosis.” Studies show 50% of patients stop taking glaucoma medications before six months, often as a result of unpleasant side effects such as ocular surface disease or poor compliance. These patients are often elderly, on medication for life and frequently with multiple topical ophthalmic drops which increases the risk of poor outcomes from other more invasive surgery.
So, there’s been a huge interest in seeking alternative technologies to help these patients. Micro-bypass glaucoma surgery (MBGS) using MIGS devices such as the iStent, increases the aqueous outflow from the trabecular meshwork. This surgery is now recognised as a safe alternative, adding significantly to the armamentarium for glaucoma treatment.
In 2019, Glaukos branched out from MIGS to enter the corneal health market with the acquisition of Avedro, maker of the first FDA-approved cross-linking technology for progressive keratoconus. Both require early referral for effective treatment. This is especially true for keratoconus, where corneal cross-linking can strengthen the cornea before it becomes too thin, staving off severe vision loss, stressed both speakers.
Keratoconic cornea changes usually start with the onset of puberty, but frequently keratoconus goes undiagnosed for a decade or more by which time major changes have occurred and the cornea may be too thin and rigid for successful cross-linking treatment.
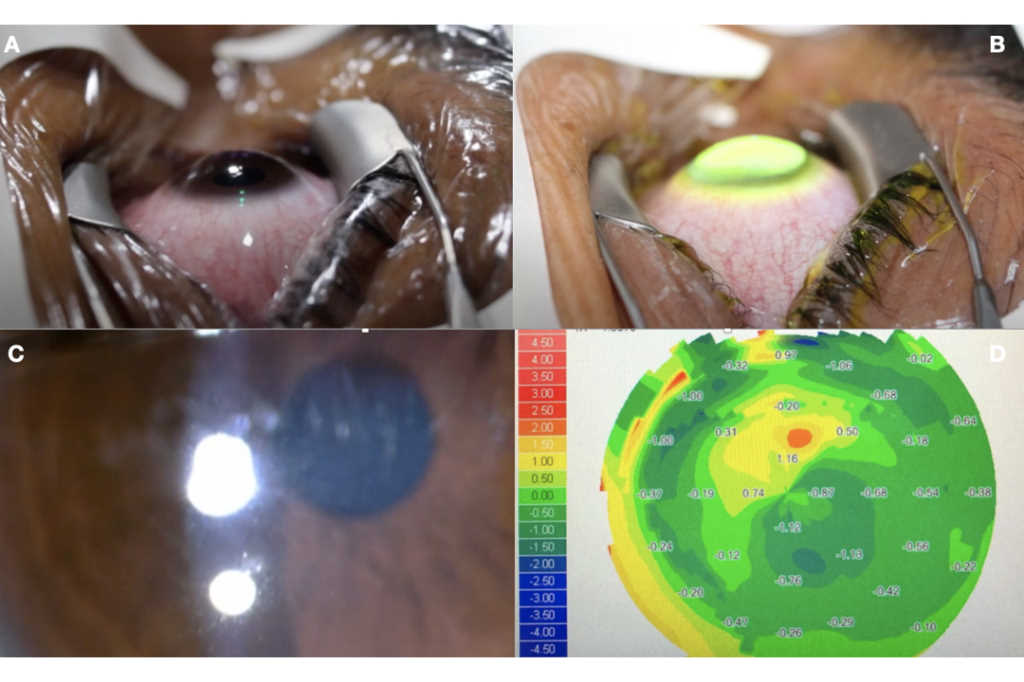
In highly allergic patients, or those with a history of corneal irregularity, Holland recommended screening children around the beginning of puberty and then six-monthly to document changes. Look at the retinoscope reflex, he said. Significant changes in astigmatism particularly large oblique cyls and a variable refraction accompanied by a drop of one or more lines of BCVA are key diagnostic indicators, together with changing corneal topography and ultimately corneal thinning if the instrumentation to measure this is available. If not, projecting a ring reflected onto the cornea, such as from a tonometer, to look for irregularity of the reflex can be helpful.
When to refer for cross-linking?
- Keratometry increase of 0.5 dioptre or more to steepest axis within a six to 12-month period
- Pachymetry 50μm or more change at the thinnest point in six to 12-month period
- Refraction cyl increase of 1D or more within six to 12 months
- Acuity drop of one or more Snellen lines in either eye. Preferably don’t wait for this!
The process of corneal cross-linking used to take a long time, but now with the ability to change intensity of the UV light, the treatment time can be shortened to well within the average teen’s music listening tolerance. It is also a minimally invasive, safe treatment with discomfort lasting about four days, for which a bandage contact lens may be helpful. Post-treatment, expect to see some corneal haze which fades over time and generally does not affect vision. Early infiltrates and haze will usually resolve quite quickly, said Holland. “The biggest challenge is keeping patients comfortable for the first few days.”
The majority of treated patients maintain the flattening of the cornea over time. Patients are best assessed for spectacles or contact lenses after three months, but most will need reassessment at six months as there can still be more flattening of the cornea.
Who’s not suitable?
If a patient’s visual acuity isn’t good with spectacles or contact lenses, there may not be improvement after treatment.
In summary, ‘get them young and keep them flat’ was the big, cross-linking take home message!
*https://eyeonoptics.co.nz/articles/archive/the-istent-evolves/
Naomi Meltzer has worked in optometry for more than 30 years. She runs an independent optometry practice specialising in low vision consultancy in Auckland and is a regular contributor to NZ Optics.