Considering glaucoma…
Ginkgo Biloba extract in ophthalmic and systemic disease, and NTG
Labkovich et al
Asia Pacific Journal of Ophthalmology: May/June 2020, volume 9, issue 3, p215-225
Supplements in glaucoma management have been a topic of interest for a long time, especially for those of us who lose sleep over patients with progressive glaucoma where the usual intraocular pressure (IOP) lowering paradigm doesn’t work. This review focused on ginkgo biloba extract (GBE) as a potential adjunctive treatment option for normal-tension glaucoma (NTG).
GBE is a leaf extract and its chemical composition can vary. Commercially available GBE consists of 60 bioactive compounds and is the sole source of about 30 of them. GBE has vasoactive, anti-inflammatory and anti-oxidative effects and also reduces blood viscosity. It has been shown to be a multifunctional neuroprotective agent as well having tumour suppression properties and is implicated in DNA repair.
Glaucoma patients taking GBE have been shown to have increased ocular blood flow. GBE supplementation suppresses steroid-induced increased IOP and reduced accumulation of extracellular materials in the cribriform layers. There is also evidence that taking GBE can improve visual field results in those with recently documented progression.
Multiple studies have reported minimal adverse effects of GBE within a specific prescribed dosage range and it is generally well tolerated. There are reports of spontaneous hyphaemia in patients taking GBE without evidence of altered blood coagulation or platelet aggregation and patients are generally asked to stop GBE prior to undergoing eye surgery.
The authors recommend that further molecular research should focus on emerging evidence of mitochondrial involvement in people with NTG compared with healthy controls.
SLT versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT)
Gazzard et al. on behalf of the LiGHT Trial Study Group
Lancet 2019; 393: 1505–16
This study, published last year by colleagues in the UK, was designed to see if selective laser trabeculoplasty (SLT) could be compared with eye drops as a first-line treatment for open angle glaucoma or ocular hypertension. From looking at the outcomes for the 718 enrolled participants, the answer was that indeed, it should be offered as an initial treatment.
This was an observer-masked, randomised controlled trial in treatment-naive patients from six UK hospitals with open angle glaucoma or ocular hypertension and no ocular comorbidities. The patients were randomly assigned to initial SLT or eye drops. An objective target IOP was set according to glaucoma severity. The primary outcome was health-related, quality of life at three years. Secondary outcomes were cost and cost-effectiveness, disease-specific, clinical effectiveness and safety.
SLT provided superior IOP stability to drops at a lower cost and, importantly, it allows almost three quarters of patients (74%) to be successfully controlled without drops for at least three years after starting treatment, so should be considered an alternative to IOP-lowering drops
This was the first direct comparison between SLT and IOP-lowering drops in a study of this type in a hospital setting, guided by a robust treatment escalation protocol to capture realistic clinical management while minimising risk of bias.
Laser peripheral iridotomy for the prevention of angle closure
Mingguang He et al
Lancet 2019 Apr 20;393(10181):1609-1618.
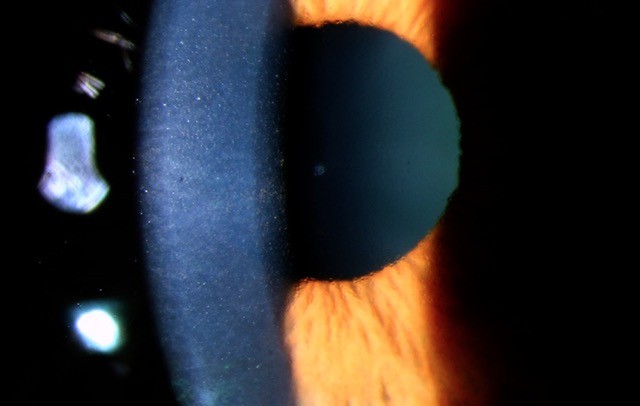
More than 75% of the 20 million people with primary angle-closure glaucoma (PACG) live in Asia; 3.1 million Chinese citizens are blind in at least one eye from PACG; and 28 million Chinese are primary angle-closure suspects (PACS). This study aimed to discover if treating PACS prophylactically with a laser peripheral iridotomy (PI) was a safe way of preventing PACG.
Also known as the Zhongshan angle-closure prevention (ZAP) study, this was a single-centre, randomised controlled trial. Nearly 12,000 screened (community-based) and 889 eligible individuals, aged between 50-70 years, were randomly assigned a laser PI in one eye. All the participants were PACS.
The primary outcome measure was incident primary angle-closure disease: elevated IOP 24mmHg or higher; peripheral anterior synechiae development; or acute angle closure over 72 months of follow-up. The incidence of the primary outcome was 4.19 per 1000 eye years in treated eyes compared with 7.97 per 1000 eye years in untreated eyes. A primary outcome event occurred in 19 treated eyes and 36 untreated eyes, and in both eyes of 10 subjects. Or, in terms of number need to treat (NNT): NNT = 44 to prevent one case of new PAC over six years; NNT = 126 to prevent one case of PACG with vision loss over 10 years
So, we can see from these results that laser PI has a modest, significant prophylactic effect. However, widespread prophylactic laser PI is not recommended because of the low rate of vision threatening outcomes. Those with PACS have a small and real risk of acute angle closure (AAC) attack, but unpredictable (increased risk if need pupil dilation). Based on the results of this study, I would recommend a patient with PACS should still have a prophylactic PI if they:
- Have PAC or PACG in the other eye
- Are geographically isolated
- Require frequent pupil dilation (diabetes)
- Have symptoms consistent with subacute angle closure
- See from only one eye
- Already have glaucoma from another mechanism
Dr Sonya Bennett is a consultant ophthalmologist with a special interest in glaucoma at Greenlane Clinical Centre and City Eye Specialists, and a senior clinical lecturer at the University of Auckland.