Trends in corneal transplantation: beyond 2020
Corneal transplantation is indicated when corneal disease or injury results in the loss of shape (keratoconus) or clarity of the cornea, usually due to oedema, scarring or protein/lipid deposition. The trends and indications for corneal grafts in New Zealand have changed dramatically over the last 30 years and four major studies from the University of Auckland (UoA) have highlighted the changing environment of corneal transplantation in New Zealand1-4. Aotearoa New Zealand has a somewhat unique pattern of corneal transplantation due to the relatively high prevalence of keratoconus. This, combined with our ageing population and major advances in keratoplasty techniques, has resulted in a rapidly evolving pattern of corneal transplantation.
First successfully performed in 19055, penetrating keratoplasty (PK) involves removing a central, typically 8mm diameter button of the host cornea and replacing it with a full-thickness donor cornea including epithelium, stroma and endothelium. Around the turn of the millennium this was the most common corneal transplantation performed1, highlighted by Edwards et al (2002), who reported the indications and types of corneal transplants performed in New Zealand from 1991-19996. The relatively high prevalence of keratoconus in Māori and Pasifika6 was the postulated reason for this being the top indication for corneal transplant during this period, followed by pseudophakic corneal oedema and regraft. The age distribution was bimodal, with two peaks in the third and eighth decades, with a mean age of 47.5 years. Interestingly, 95% of transplants performed were PKs, with the exception being a very small number of lamellar keratoplasties. During the study period New Zealand’s population was 3.75 million, and approximately 175 corneal transplants were performed per year1.
Deep anterior lamellar keratoplasty (DALK) has been performed in small numbers in New Zealand since the late 1990s for the treatment of corneal diseases with normal-functioning endothelium (Fig 1). This involves transplanting only donor anterior stroma and epithelium onto a bed of host Descemet’s membrane and endothelium with residual posterior stroma7. Initial transplantation techniques using ‘stroma only’ without endothelium actually began 150 years ago, but were only perfected in the last 30 years8.
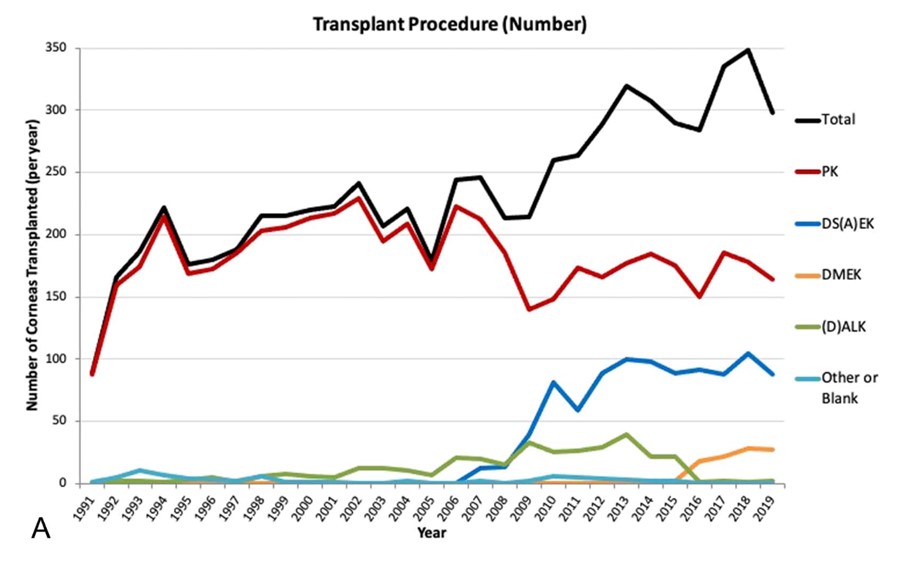
Fig 1. Types of corneal transplant performed in New Zealand 1991-20194
Cunningham et al (2012) examined 10 years of transplants from 2000-2009 and found an increasing number of DALKs being performed. In the same time period, a small number of Descemet’s stripping endothelial keratoplasties (DSEK) were also performed for the treatment of corneal endothelial diseases2. DSEK is a partial thickness graft in which the donor endothelium, Descemet’s membrane and a thin layer of posterior stroma replace the host endothelium and Descemet’s membrane7. This technique was introduced to New Zealand in 2007 and offers several advantages over PK2,7. As less donor stroma and no epithelium is transplanted, there is less risk of rejection; there is also decreased operative risk as it is less invasive. It also enables quicker visual recovery7.
In spite of these benefits of DSEK, the uptake of this technique was relatively slow within New Zealand, as noted by Cunningham et al. This could be due to a proportionally high number of severe keratoconus with delayed presentation, such that the only treatment option was PK. In 2000-2009, the primary indication for corneal grafts remained keratoconus (41%), but regraft became the second most common indication. Also notable from this study was a significant increase in the overall number of transplants performed, rising 30% from an average of 170 in the previous decade to an average of 220 per year. The authors felt this was likely due to increased eye donation efforts coordinated by the New Zealand Eye Bank, a larger number of sub-specialised corneal surgeons in the country and a growing population2.
By 2015, Kim et al (2016) identified that 31% of corneal transplants were DS(A)EK, with the other 60% being PKs3. In 2015 Descemet’s membrane endothelial keratoplasty (DMEK) was more widely introduced to New Zealand3,4. This newest partial-thickness graft involves transplanting only Descemet’s membrane and endothelium. This procedure has a lower risk of rejection than DSEK due to the absence of donor stromal tissue7. Although the review took place prior to this new technique’s impact in New Zealand, the authors note its significant uptake in the US and predict a stronger move away from PK with time.
The number of transplants performed over the entire period from 1991-2015 was found to increase steadily at a rate of 23 additional corneal transplants per year. Notably, the population receiving corneal transplants began to shift, with decreasing transplants for those aged less than 40 years and an increase in those over 40 years, but the age distribution remained bimodal. Keratoconus remained the primary indication for corneal grafts but with an increasing number of re-grafts from 2011-20153, possibly explained by the progressive failure of penetrating keratoplasties performed 20-30 years earlier6. Interestingly, the third most common indication became Fuch’s endothelial corneal dystrophy, the reason postulated being the availability of improved diagnostic tools and the rapid recovery following endothelial keratoplasty, making early diagnosis and treatment possible3.
A 2021 New Zealand study by Chilibeck et al examined corneal transplantation trends over 30 years, from 1991-2020, specifically addressing changes over the most recent five years4. Twenty years since initial studies, the mean age of transplantation remained unchanged at 50 years, but the most common recipient age group was 20-39 years. For the first time, regrafts overtook keratoconus as the most common primary indicator for corneal grafts4, as shown in Fig 2. One explanation for this major change was the introduction of corneal crosslinking (CXL), a procedure introduced to the country in 2007, with significant success in treating early-stage keratoconus and preventing progression.



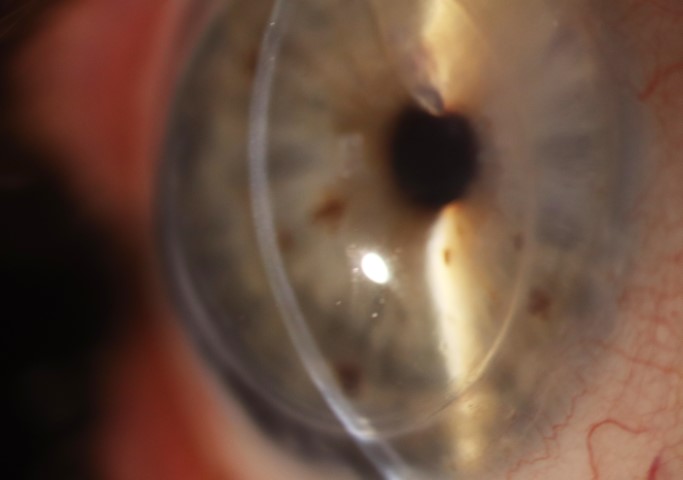
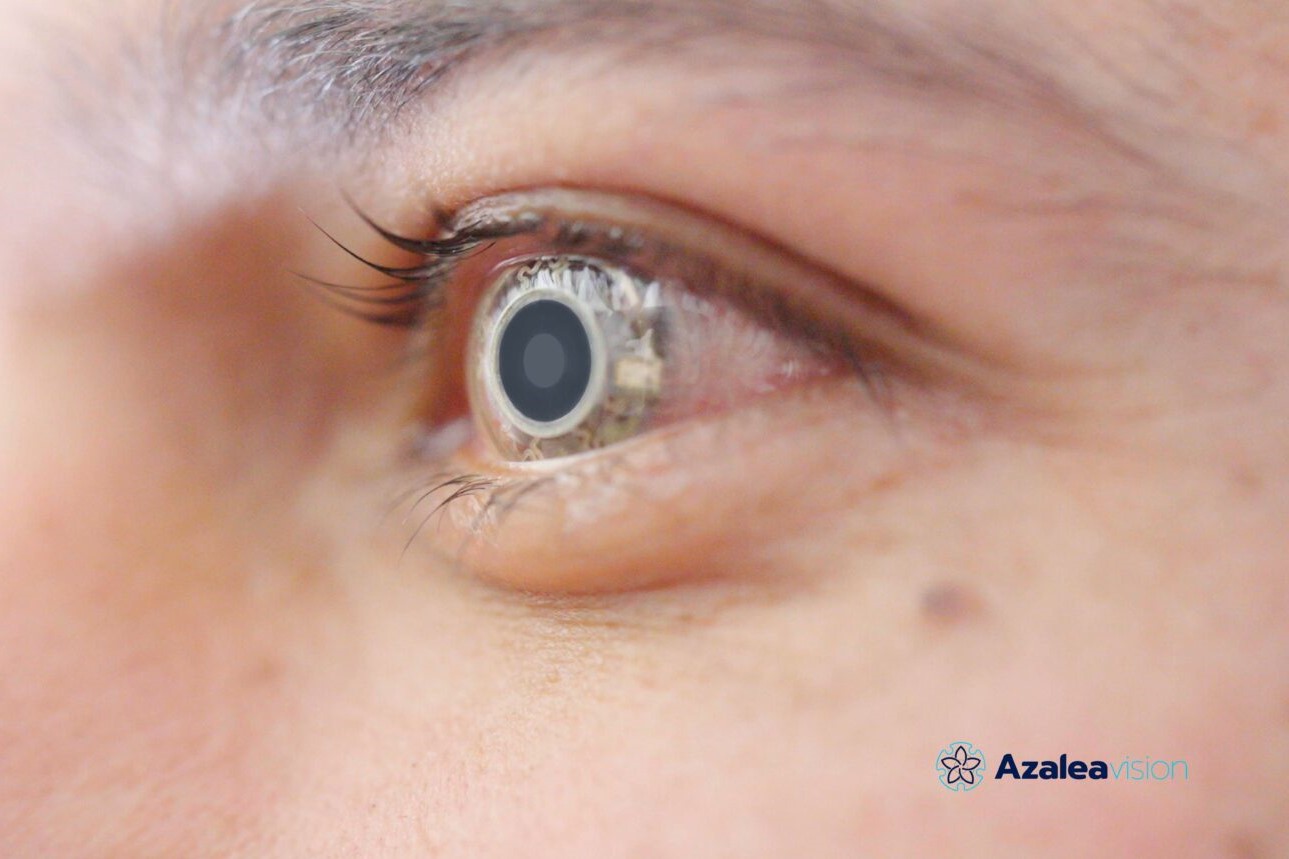
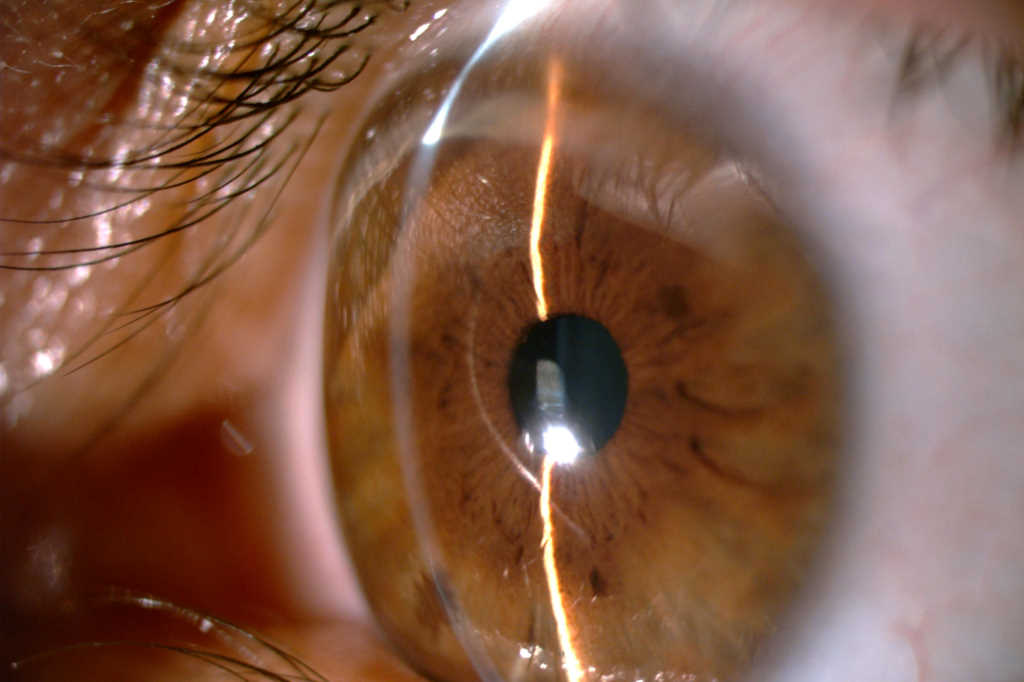
Fig 2. Clockwise from top left: A) Crystal-clear penetrating keratoplasty for advanced keratoconus at three months post-surgery with BCVA of 6/12. B) A decompensated penetrating corneal transplant awaiting an endothelial keratoplasty regraft. C and D show the same cornea as in B at three months following a DSAEK, highlighting a clear cornea and extremely thin posterior DSAEK with 6/6 visual acuity
CXL has become widely practiced, enabling the treatment of mild to moderate keratoconus and mitigating the need for a corneal graft in many patients. Combined with a concerted nationwide effort to identify and treat keratoconus as early as possible, CXL has moved us away from end-stage treatment such as corneal transplantation and further towards preventative measures6. Therefore, the proportion of PKs is expected to drop further in coming years in relation to the reduced need for surgical interventions for keratoconus. Alongside this is the aforementioned increase in the ages of corneal transplantation candidates nationwide, with many transplants reaching the natural end of their lifespan since the initial 1994 boom of corneal grafts due to endothelial exhaustion, rejection and recurrent peripheral ectasia1, hence the ever-growing need for regrafts.
Also of note is the gradual downward trend in indications for grafts for pseudophakic bullous keratopathy and keratitis. In the 1990s, over a quarter of all grafts were performed for bullous keratopathy and 15% for keratitis; by 2020 this indication had dropped to approximately 6% for both1,4. As predicted and observed in earlier studies, the proportion of grafts which were PKs continued to decrease; by 2020, only around half of the grafts performed were PKs, the remainder being lamellar. Interestingly, the percentage of DSAEK remained stable over the past 10 years or so, but the newer technique DMEK became more widely performed4 (currently with a ratio of approximately 4:1, unpublished data).
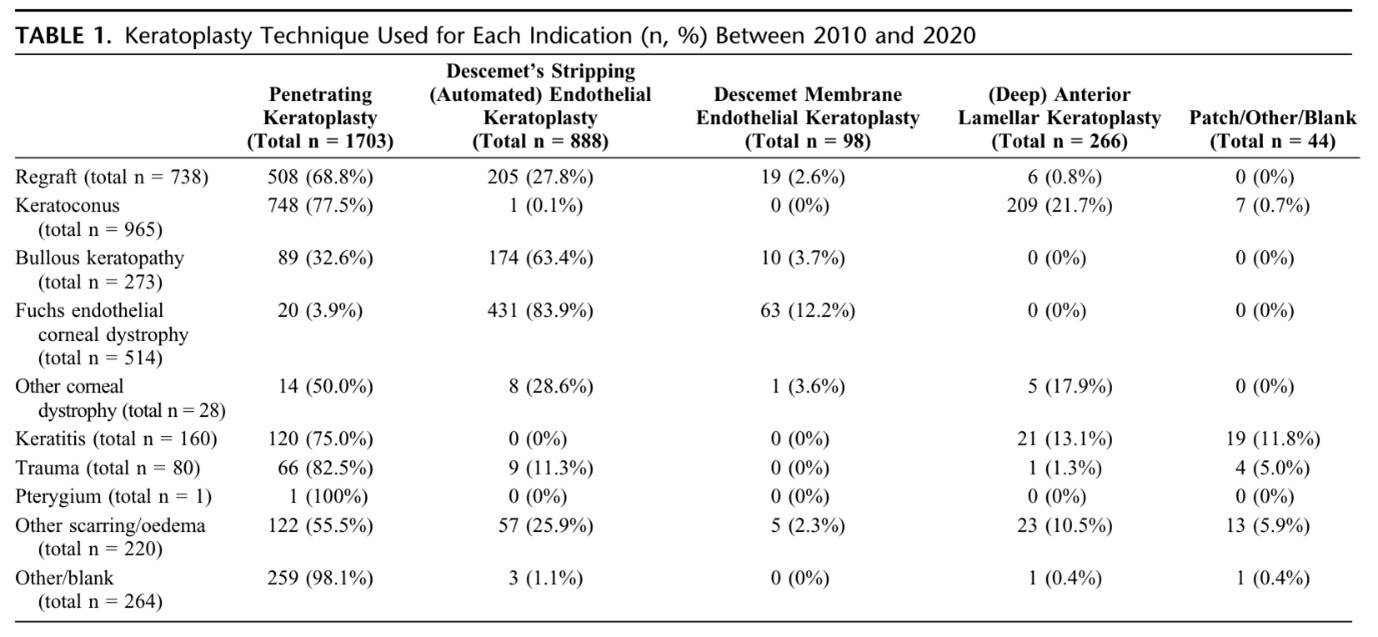
Table 1. Keratoplasty technique used for each indication between 2010 and 20204
As the surgical techniques in corneal transplantation continue to develop and refine, so too do the populations and pathologies being treated. The landscape of corneal transplantation within New Zealand has shifted seismically in recent decades, with more progress and change likely since the Covid-19 pandemic. The Department of Ophthalmology, UoA continues to partner with, collate and publish New Zealand National Eye Bank data to continue and progress this research area which is so important in Aotearoa.
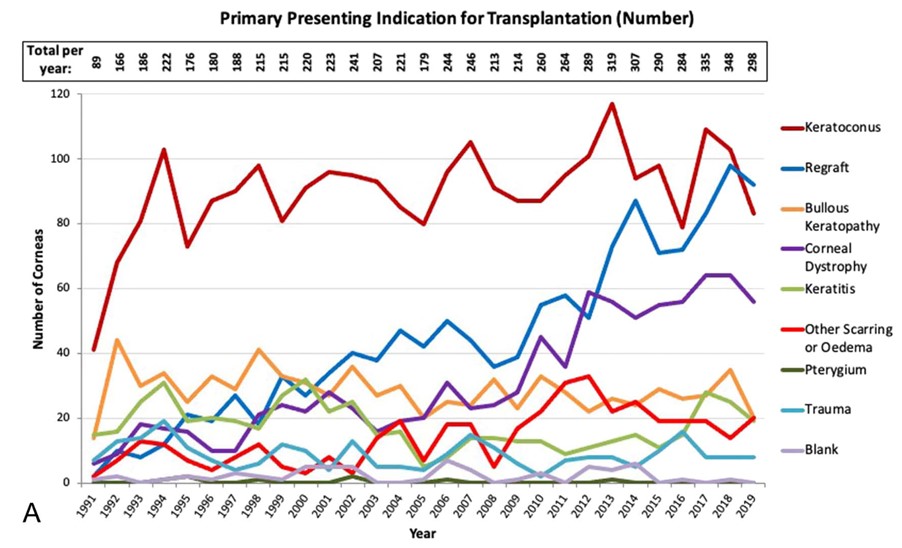
Fig 3. Indication for corneal transplant performed in New Zealand 1991-2019 with a recent
decreasing trend in keratoconus as an indication and increase in regraft4
References
1. Edwards M, Clover G, Brookes N, Pendergrast D, Chaulk J, McGhee C. Indications for corneal transplantation in New Zealand: 1991-1999: Cornea. 2002;21(2):152-155.
2. Cunningham W, Brookes N, Twohill H, et al. Trends in the distribution of donor corneal tissue and indications for corneal transplantation: the New Zealand National Eye Bank Study 2000-2009. Clin Experiment Ophthalmol. 2012;40(2):141-147.
3. Kim B, Meyer J, Brookes N, et al. New Zealand trends in corneal transplantation over the 25 years 1991-2015. Br J Ophthalmol. 2016;101.
4. Chilibeck C, Brookes N, Gokul A, et al. Changing trends in corneal transplantation in Aotearoa/New Zealand, 1991 to 2020: effects of population growth, cataract surgery, endothelial keratoplasty, and corneal cross-linking for keratoconus. Cornea. 2022;41(6):680-687.
5. Zirm E. Eine erfolgreiche totale keratoplastik (A successful total keratoplasty). Refract Corneal Surg. 1989;5(4):258-261.
6. Gokul A, Ziaei M, Mathan J, et al. The Aotearoa research into keratoconus study: geographic distribution, demographics, and clinical characteristics of keratoconus in New Zealand. Cornea. 2022;41(1):16-22.
7. Tan D, Dart J, Holland E, Kinoshita S. Corneal transplantation. The Lancet. 2012;379(9827):1749-1761.
8. Crawford A, Patel D, McGhee C. A brief history of corneal transplantation: From ancient to modern. Oman J Ophthalmol. 2013;6(Suppl 1):S12-S17.

Dr Natalie Allen is a Maurice and Phyllis Paykel Trust corneal research fellow, working with Prof McGhee and pursuing a PhD on corneal transplantation at the University of Auckland (UoA).

Dr Akilesh Gokul is an optometrist and a senior lecturer in UoA’s Dept. of Ophthalmology. A clinician-scientist, his main research interests include keratoconus, contact lenses, crosslinking and inequity in healthcare – knowledge he employs through his work with Te Whatu Ora’s public crosslinking service.

Dr Jie Zhang is a senior HRC research fellow and scientist in the Dept. of Ophthalmology, UoA. She has specific research interests in both laboratory and clinical aspects of the cornea and anterior segment.